Treatment of Pneumothorax with a Portable Thoracic Vent
The Case
A 59 year-old male who underwent a same-day bronchoscopy with transbronchial biopsies taken for diffuse parenchymal lung disease presents later that afternoon to the Emergency Department with a chief complaint of shortness of breath.
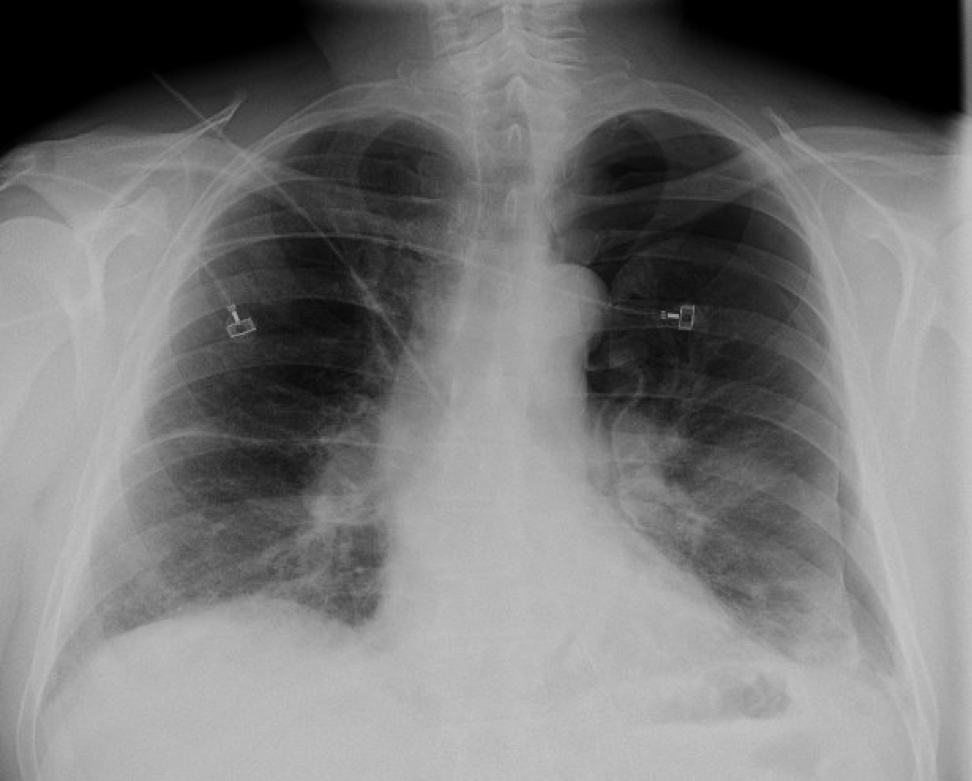
Upon arrival he is noted to be mildly tachypneic with a respiratory rate of 22. He is not hypoxic and the remainder of his vital signs are within normal limits. Exam reveals diminished breath sounds in the left lung fields. An upright chest x-ray demonstrates a large left-sided pneumothorax (Figure 1).
Figure 1: Initial chest x-ray demonstrating large left-sided pneumothorax
Discussion
The conventional treatment of a spontaneous or iatrogenic pneumothorax is with a small-bore thoracostomy tube also known as a pigtail catheter. This usually requires connecting the patient to an underwater seal device such as a pleuravac, thereby necessitating admission to the hospital for monitoring. However, there are other devices available to treat this condition that can be deployed more rapidly and with similar success rates. In some cases, patients treated with these devices do not even require hospitalization.
One such device is the Tru-Close thoracic vent. The Tru-Close (also referred to as a Thora-Vent) is a portable device that consists of an 11 or 13 French catheter connected directly to a small air chamber containing a one-way valve and self-sealing port.
Using either an over-the-wire Seldinger technique or a trocar for direct insertion, the catheter is inserted using local anesthetic and sterile technique into the affected side at the patient’s second intercostal space on the mid-clavicular line (similar in location to where one would needle decompress a tension pneumothorax). The entire device is then affixed to the chest wall with adhesive wings. It can be left to air seal or connected to suction if clinically indicated. Time to complete the entire procedure from beginning to end takes around one minute (a video with more information on The Tru-Close, as well as the procedure for placement can be found here).
The literature on the use of thoracic vent devices in treatment of pneumothorax is limited. In one study of 18 patients (15 with spontaneous pneumothorax and 3 with iatrogenic pneumothorax), 88.9% of patients (16/18) treated with a Tru-Close thoracic vent had complete lung re-expansion within 24 hours. All of the patients with spontaneous pneumothorax were discharged to follow up as an outpatient. There were no immediate complications, and most patients remained recurrence free during a three-year follow up period. It is important to note that in this study, the device was inserted under fluoroscopic guidance, something that is not readily available to most emergency physicians.
In another study of 30 patients comparing thoracic vent devices to conventional intercostal tube drainage, the authors found that there was no significant difference in the rates of lung reexpansion or complications between the two groups. They did find that patients treated with the thoracic vent devices needed significantly less analgesics than patients treated in the conventional manner. Furthermore, 70% of patients treated with a thoracic vent were managed as an outpatient, whereas all patients treated with the conventional intercostal tube required admission.
This literature suggests that in reliable, otherwise healthy patients who present with an uncomplicated spontaneous pneumothorax, the use of a thoracic vent device for lung reexpansion may be a good option that could potentially enable the patient to be discharged and managed as an outpatient provided they have close follow-up. Patients generally tolerate the device well as allows maximum ambulation while device in place.
Case Resolution
A Tru-Close thoracic vent is placed in the emergency department, and a repeat chest x-ray demonstrates rapid resolution of the pneumothorax (Figure 2). The patient is admitted to the medical service due to a persistent air leak. He has an uneventful hospital stay and is discharged on hospital day 3.
Figure 2: Interval resolution of left-sided pneumothorax after placement of a Tru-Close thoracic vent.
Faculty reviewer: Kristina McAteer
References
Kim et al. “Effectiveness of Ambulatory Tru-Close Thoracic Vent for the Outpatient Management of Pneumothorax: A Prospective Pilot Study.”Korean J Radiol. 2017 May-Jun;18(3):519-525. doi: 10.3348/kjr.2017.18.3.519. Epub 2017 Apr 3.
Roggla, et al. “The management of pneumothorax with the thoracic vent versus conventional intercostal tube drainage.” The Central European Journal of Medicine. 1996;108(11):330-3.
Tsuchiya et al. “Outpatient Treatment of Pneumothorax with a Thoracic Vent: Economic Benefit.” Respiration. 2015;90(1):33-9. doi: 10.1159/000381958. Epub 2015 May 12.