Keep Your Eye on the Target: POCUS for Intussusception
Faculty Reviewer: Erika Constantine, MD
Case:
HPI: An 18 month old previously healthy female with a history of mild intermittent constipation, but no prior abdominal surgeries presented to the ED with 3 days of non-bilious, non-bloody emesis and abdominal pain not responsive to laxatives and Zofran. On the day of presentation she developed multiple episodes of screaming associated with grabbing her stomach and pulling up her legs. Episodes lasted for 30 seconds to 1 minute and self-resolved. She was afebrile. Oral intake and urine output were decreased, and she had no stools on the day of presentation. Her last bowl movement was 1 day prior to presentation and was loose without blood. The patient had nasal congestion and rhinorrhea the prior week.
Vitals: Pulse 124 | Temp 98.7 °F (37.1 °C) | Resp 26 | Wt 15.7 kg | SpO2 98%
Exam: Unremarkable with the exception of diffuse abdominal tenderness and voluntary guarding, but no rebound. No hepatosplenomegaly was appreciated. Bowel sounds were diminished.
Given the story and exam, the clinical suspicion for intussusception was high, and an initial two view abdominal x-ray was obtained:
Figure 1: Abdominal Xrays
2 View Abdominal x-ray revealed a soft tissue mass in the right upper quadrant concerning for intussusception (arrows). A comprehensive ultrasound confirmed ileocolic intussusception.
A bedside point-of-care ultrasound was performed while patient was awaiting comprehensive radiographic evaluation. A donut-shaped mass was visualized in the right lower quadrant, consistent with ileo-colic intussusception.
Figure 2a: Cross-sectional view of a donut-shaped mass, consistent with intussusception
Figure 2b: Longitudinal view of the intussusception
The patient underwent a successful air-enema reduction. Post air reduction, the left lateral decubitus film shows resolution of the paucity of gas previously seen in the RUQ.
Figure 3: Post reduction xray
Epidemiology of Intussusception:
Intussusception is the most common abdominal emergency in early childhood, particularly among children younger than 2 years of age. Approximately 60% of children with intussusception are less than 1 year old and 80-90% are less than 2 years old. Additionally, it is the most common cause of intestinal obstruction in infants between 6 and 36 months and there is a slight male predominance, with a male:female ratio of approximately 3:2.
Intussusception in this age group most often occurs at the ileocecal junction, leading to ileocolic intussusception. The intussusceptum, a proximal segment of bowel, telescopes into the intussuscipiens, a distal segment.
Approximately 75 percent of cases of intussusception in children are considered to be idiopathic because there is no clear disease trigger or pathological lead point. Mesenteric lymph nodes may act as a lead point and may occur in the setting of gastroenteritis (both viral and bacterial), viral upper respiratory illnesses, flu-like illnesses, and adenovirus. Henoch-Schönlein purpura, HSP, is also associated with intussusception, but more commonly ileo-ileal. Non-infectious causes of lead points include Meckels, polyps, tumors (lymphoma), hematomas, vascular malformations, duplication cysts, and post-operative scarring.
Clinical Features:
The classic presentation of intussusception includes sudden onset intermittent, severe, crampy, and progressive abdominal pain, accompanied by inconsolable crying and drawing up the legs towards the abdomen, with return to baseline between episodes. As lethargy may follow episodes of abdominal pain, intussusception should be on the differential diagnosis for any young child presenting with unexplained lethargy or altered mental status. Non-bloody, non-bilious emesis is often present. The classically described triad of pain, palpable abdominal mass, and currant jelly stool occurs in <15% of children.
Imaging Techniques:
Abdominal plain films: A two view abdominal x-ray can be used to evaluate the bowel gas pattern and to exclude perforation in patients with suspected intussusception. It is not the imaging method of choice, as a negative plain film cannot rule out intussusception. A plain film is less sensitive and specific than ultrasonography for intussusception, but may include the following suggestive findings:
Signs of intestinal obstruction (distended loops of bowel with absence of colonic gas)
Target sign (two concentric circles superimposed on the right kidney)
Crescent sign (soft tissue density projecting into the gas of the large bowel)
Obscured liver margin (as seen in the patient in this vignette)
Lack of air in the cecum
Pneumoperitoneum (RARE, secondary to perforation)
Ultrasonography: Abdominal ultrasound is the modality of choice, with sensitivity and specificity approaching 100% when performed by experienced ultrasonographers. The classic imaging findings include a “target sign” or “bull’s eye” that occurs due to the layers of intestines within one another. This target is usually ≥3 cm in diameter.
Figure 4: Cross sectional view of intussusception
Figure 5: Longitudinal view of intussusception
Point of Care US (POCUS) for Intussusception:
Bedside ultrasound may lead to more expeditious diagnosis, particularly when pediatric radiology is not available, and may facilitate more rapid comprehensive radiographic and/or surgical evaluation. A 2011 study showed that 6 PEM physicians could perform the exam with a sensitivity of 85%, specificity of 97%, positive predictive value of 85%, and negative predictive value of 97% for diagnosing intussusception after just a 1 hour course!
Diagnostic pitfalls with ultrasonography include enlarged lymph nodes, non-pathologic ileo-ileal intussusception, the psoas muscle, colonic stool, and the kidneys, all of which may be misinterpreted as intussusception. Scan the entire abdomen and try to localize the actual kidneys. Confirm that the depth of the image and the diameter of the findings in question are consistent with the typical intussusception parameters, and observe for surrounding peristalsis to help decrease misinterpretation of findings.
Ultrasound Technique:
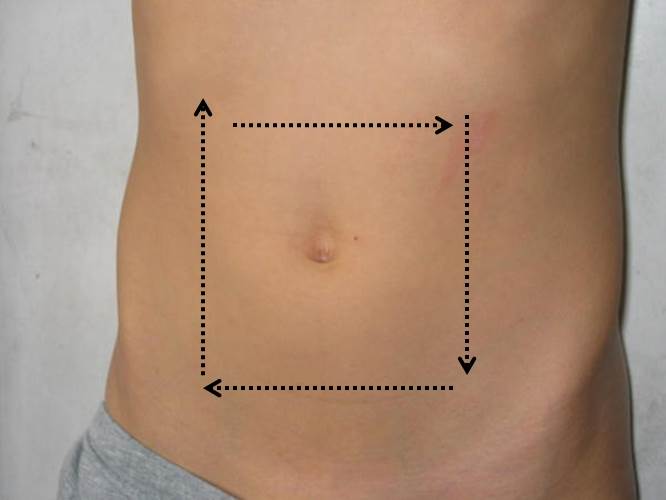
Using a linear probe, start by placing the probe transversely in the RLQ and attempt to identify the psoas muscle (semicircular structure with striations and iliac vessels just medial to it). Set the depth to at least 6 cm. Slowly sweep superolaterally until the liver and gallbladder are visualized. Proceed along the course of the large bowel as the intussusception may be seen in the LLQ. If seen, an intussusception should be imaged in two planes.
Figure 6: Ultrasound technique
Treatment:
The preferred method of treatment for intussusception is nonoperative, with air or barium enema reduction, which is performed by radiology. Surgery should be close by in case of complication and/or need for urgent operative intervention. Operative intervention may be needed if non-operative reduction fails or if there is concern for a mass lesion as the pathological lead point, or if there is suspected or proven bowel perforation or necrosis.
Faculty Reviewer: Dr. Erika Constantine
References:
1. KitagawS, Miqdady M. Intussusception in children. Uptodate.com. Accessed April 17, 2016. <http://www.uptodate.com/contents/intussusception-in-children source=search_result&search=intussusception&selectedTitle=1~102>.
2. Doniger SJ, Salmon M, Lewiss RE. Point-of-Care Ultrasonography for the Rapid Diagnosis of Intussusception: A case series. Pediatr Emergency Care. 2016 Feb 15. Epub ahead of print. PMID: 26890297.
3. Alletag MJ, Riera A, Langhan ML, Chen L. Use of emergency ultrasound in the diagnostic evaluation of an infant with vomiting. Pediatr Emerg Care. 2011, Oct; 27(10):986-9.
4. Eshed I, Gorenstein A, Serour F, et al. Intussusception in children: can we rely on screening sonography performed by junior residents? Pediatr Radiol. 2004;34;134-137.
5. Ramsey KW, Halm BM. Diagnosis of intussusception using bedside ultrasound by a pediatric resident in the emergency department. Hawaii J Med Public Health. 2014 Feb;73(2):58-60.
6. Riera A, Hsiao AL, Langhan ML, Goodman TR, Chen L. Diagnosis of intussusception by physician novice sonographers in the emergency department. Ann Emerg Med. 2012 Sep;60(3):264–268. [PubMed].
7. Chang YJ, Hsia SH, Chao HC. Emergency medicine physicians performed ultrasound for pediatric intussusceptions. Biomed J. 2013 Jul-Aug;36(4):175–178. [PubMed].
8. Halm BM. Reducing the time in making the diagnosis and improving workflow with point-of-care ultrasound. Pediatr Emerg Care. 2013 Feb;29(2):218–221. [PubMed].