A Screwy Case of Pediatric Shortness of Breath
“Airway foreign bodies (FB) are a common complaint in the pediatric populatioN…”
Introductory Case
A 5-year-old female presents with chest pain and shortness of breath for the past 12 hours. She was found to be choking the evening prior, and the “Heimlich” maneuver was applied to her chest, resolving the choking episode. Since that time, she has been complaining of chest pain and shortness of breath. She was able to eat breakfast and has had no dysphagia or odynophagia. She was seen by her pediatrician and was sent directly to the emergency department for hypoxia.
Vital signs: T 37.2°C, HR 118, BP 104/53, RR 32, SpO2 86% RA (improved to 97% on 4L NC).
On examination in the Emergency Department, she is well appearing, tachypnic, but in no respiratory distress, and has no voice change or audible respiratory sounds. There are normal breath sounds throughout the right chest. Breath sounds are absent on the left. The trachea is midline, and there is no crepitus.
The history and examination is highly suspicious for an aspirated foreign body, but there is also concern for pneumothorax and hemothorax, especially given the report of an improperly applied Heimlich maneuver to the chest.
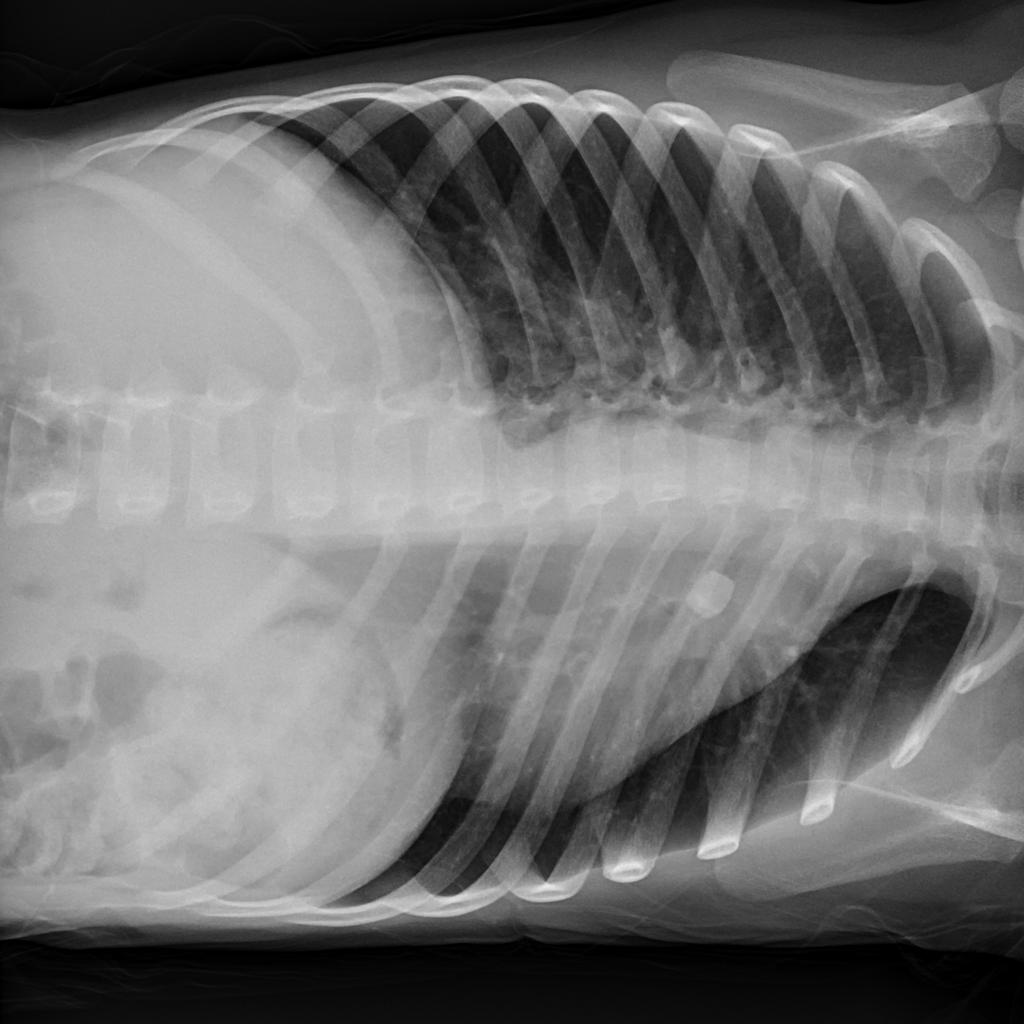
The following chest x-ray was obtained:
Figure 1: Upright AP Chest radiograph demonstrating a foreign body at the level of the carina
Discussion
Airway foreign bodies (FB) are a common complaint in the pediatric population. Infants and toddlers explore the world around them by putting objects into their mouths, so it is unsurprising that children aged 6 months to 3 years are the most common age group to present with choking or a concern for FB aspiration. Younger children are at increased risk for significant airway obstruction because of their narrow airways. Their underdeveloped communication skills and unreliable histories further complicate clinical scenarios.
Laryngotracheal FBs are most likely to present with acute respiratory distress, hoarseness, or stridor. Bronchial FBs are more likely to present with coughing, wheezing, diminished breath sounds, pain, shortness of breath, or infectious symptoms. Children frequently present with only mild symptoms.
Management of airway, breathing, and circulation are of immediate concern in children who appear distressed. This may include application of the Heimlich maneuver or back blows in older children and infants, respectively, as well as FB removal under direct visualization. Children who are unable to protect their airways, adequately oxygenate, or effectively ventilate may require placement of an advanced airway.
Radiography is the primary modality used for the identification of foreign bodies, and AP/PA and lateral chest films, as well as soft tissue neck views, are the primary workhorse. The ability of an x-ray to identify an object depends on two distinct concepts: radiopacity and radiographic visibility. Radiopacity is an intrinsic feature of all objects and is a measurement of their ability to either absorb or scatter x-rays. Radiographic visibility depends upon radiopacity but is affected by the size/density of the object, anatomic location, surrounding tissues/structures, and body habitus. As such, radiolucent objects may be radiographically visible.
Many FBs are radiolucent and may have poor radiographic visibility, resulting in negative x-rays; therefore, if there is high suspicion for FB, further investigation should be pursued. In the setting of radiographs negative for FB, secondary signs such as shifting of the mediastinum, abnormal heart shadows, emphysema, atelectasis, and consolidation may help with diagnosis. Delayed presentations may be further missed and diagnosed simply as pneumonia or asthma. As such, when either is unresponsive to traditional treatments, missed FB should be considered.
Additional radiographic views have been traditionally used to help identify FBs not otherwise apparent on standard views. These include left and right lateral decubitus and inspiratory/expiratory views. Expiratory films are most helpful in cooperative patients and seek to identify air trapping at end-expiration. Decubitus films help to identify differential air trapping. In patients without a FB, the dependent lung is relatively underinflated. When this is not present, or there is hyperlucency, it suggests air trapping due to a one-way valve effect (see figure 1). Although commonly used, studies have found that the use of decubitus films actually decreases the specificity of standard chest x-ray without changing the sensitivity, suggesting they may be little diagnostic value with the added risk of increased radiation exposure.
Figure 2:
Figure 2: Right lateral decubitus (Courtesy of Jeremy Jones, radiopedia.org)
Figure 3: Left lateral decubitus (Courtesy of Jeremy Jones, radiopedia.org)
Rigid bronchoscopy is both diagnostic and therapeutic. It is the most common method of FB removal. Flexible bronchoscopy is generally more appropriate in situations where there is some suspicion for a FB, but a poorly suggestive history and examination. Rigid bronchoscopy should always be performed in situations where there are clear findings and a history as to suggest FB aspiration, even in the absence of normal radiographs, as radiographs as the least sensitive within the first 24 hours after aspiration, especially when assessing for secondary findings.
Missed and subsequently retained FBs are associated with a number of complications, including: pneumonia, lung abscess, bronchiectasis, atelectasis, and increased granulation tissue of the surrounding airways. If there is evidence of infection, such as a post-obstructive pneumonia, empiric antibiotics with anaerobic coverage should be started, even if the FB is removed.
Case Conclusion
The patient was taken to the OR by pediatric surgery where the foreign body was removed to the level of the vocal cords by bronchoscopy and then removed under direct visualization by Macgill forceps. She did well postoperatively but was given a dose of dexamethasone to prevent worsening airway swelling. After an evening of monitoring and a repeat CXR which demonstrated no evidence of pneumonia or remaining atelectasis, she was discharged the next day.
Faculty Reviewer: Jane Preotle, MD
References & Further Readings
Assefa, D., Amin, N., Stringel, G., & Dozor, A. J. (2007). Use of decubitus radiographs in the diagnosis of foreign body aspiration in young children. Pediatr Emerg Care, 23(3), 154-157. doi:10.1097/PEC.0b013e3180328cd8
Black, R. E., Johnson, D. G., & Matlak, M. E. (1994). Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg, 29(5), 682-684.
Brown, J. C., Chapman, T., Klein, E. J., Chisholm, S. L., Phillips, G. S., Osincup, D., . . . Bittner, R. (2013). The utility of adding expiratory or decubitus chest radiographs to the radiographic evaluation of suspected pediatric airway foreign bodies. Ann Emerg Med, 61(1), 19-26. doi:10.1016/j.annemergmed.2012.05.026
Cohen, S., Avital, A., Godfrey, S., Gross, M., Kerem, E., & Springer, C. (2009). Suspected foreign body inhalation in children: what are the indications for bronchoscopy? J Pediatr, 155(2), 276-280. doi:10.1016/j.jpeds.2009.02.040
Gang, W., Zhengxia, P., Hongbo, L., Yonggang, L., Jiangtao, D., Shengde, W., & Chun, W. (2012). Diagnosis and treatment of tracheobronchial foreign bodies in 1024 children. J Pediatr Surg, 47(11), 2004-2010. doi:10.1016/j.jpedsurg.2012.07.036
Green, S. S. (2015). Ingested and Aspirated Foreign Bodies. Pediatr Rev, 36(10), 430-436; quiz 437. doi:10.1542/pir.36-10-430
Rodriguez, H., Passali, G. C., Gregori, D., Chinski, A., Tiscornia, C., Botto, H., . . . Cuestas, G. (2012). Management of foreign bodies in the airway and oesophagus. Int J Pediatr Otorhinolaryngol, 76 Suppl 1, S84-91. doi:10.1016/j.ijporl.2012.02.010
Tseng, H. J., Hanna, T. N., Shuaib, W., Aized, M., Khosa, F., & Linnau, K. F. (2015). Imaging Foreign Bodies: Ingested, Aspirated, and Inserted. Ann Emerg Med, 66(6), 570-582 e575. doi:10.1016/j.annemergmed.2015.07.499
Wiseman, N. E. (1984). The diagnosis of foreign body aspiration in childhood. J Pediatr Surg, 19(5), 531-535.