Diving Deep: Pulmonary Barotrauma in a Free Diver
Case
A 24-year-old male presented to the Emergency Department with cough and hemoptysis. The patient had been spearfishing when his symptoms began. The patient had dove to a depth of 50 feet using 11 lbs of weights on his belt, holding his breath along the way. On the way to the surface, he developed chest pain. After getting onto the boat, the patient coughed up approximately 5 tablespoons of bright red blood. After feeling a bit better, he went down again to a depth of 30 feet in order to catch a large fish. After returning to his boat, the patient was still experiencing cough, pleuritic chest pain, and mild shortness of breath.
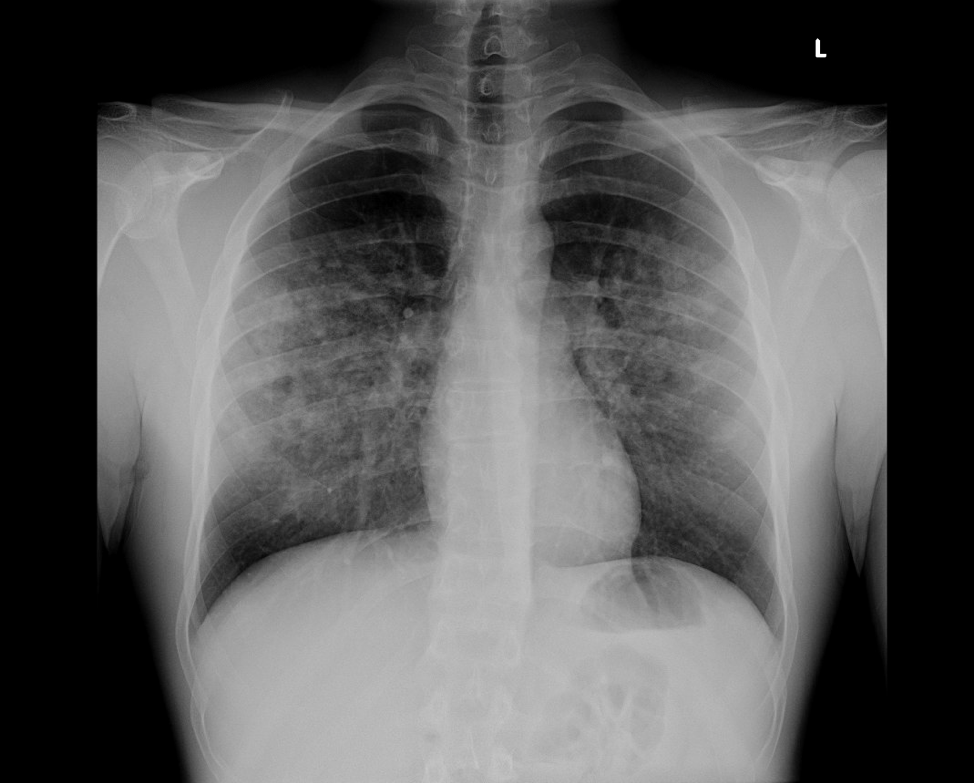
On arrival to the emergency department, the patient was breathing comfortably on room air. He did not complain of any headache, visual changes, ear pain, nausea, joint or muscle pain, or any other symptoms. On exam, he was comfortable and his lungs were clear to auscultation bilaterally. The patient had no further hemoptysis after arrival to the emergency department. Given the patient’s chest pain and subjective shortness of breath, a chest x-ray was performed.
Chest X-ray notable for patchy, bilateral, midlung predominant airspace disease.
The patient was placed on supplemental oxygen and was admitted to the medical ICU for close monitoring overnight. Pulmonology was consulted who recommended supportive care and repeat chest x-ray the following day. A CT scan of the chest was preformed to evaluate for any underlying pulmonary parenchymal disorders.
Single image from chest CT scan showing bilateral patchy airspace disease
A chest x-ray was completed the following morning in the medical ICU.
Chest X-ray notable for grossly stable, patchy bilateral airspace disease that is midlung predominant.
The patient remained hemodynamically stable and without respiratory distress throughout his hospitalization. He was discharged home on hospital day #2.
BACKGROUND PHYSICS
Spearfishing may be done while freediving, snorkeling or SCUBA diving. Our patient and his friends were freediving, or breath-hold diving. Unlike SCUBA diving, breath-hold divers do not use supplemental air underwater. Divers face a unique set of underwater hazards in addition to the general aquatic problems; such as drowning, hypothermia, water-borne infectious diseases, and interactions with hazardous marine life. When diving deep, free divers are exposed to increased pressure, causing a spectrum of injuries to the body.
Pressure contributes either directly or indirectly to the majority of serious diving-related medical problems. As a diver descends underwater, absolute pressure increases much faster than in air. The pressure change with increasing depth is linear, although the greatest relative change in pressure per unit of depth change occurs nearest the surface, where it doubles in the first 33 feet of sea water. The body behaves as a liquid and follows Pascal’s law; pressure applied to any part of a fluid is transmitted equally throughout the fluid. When a diver submerges, the force of the tremendous weight of the water above is exerted over the entire body. The body is relatively unaware of this change in pressure.
Pascal’s Law: pressure applied to any part of a fluid is transmitted equally throughout the fluid.
Source: https://upload.wikimedia.org/wikipedia/commons/thumb/2/27/Pascals-law.svg/2000px-Pascals-law.svg.png
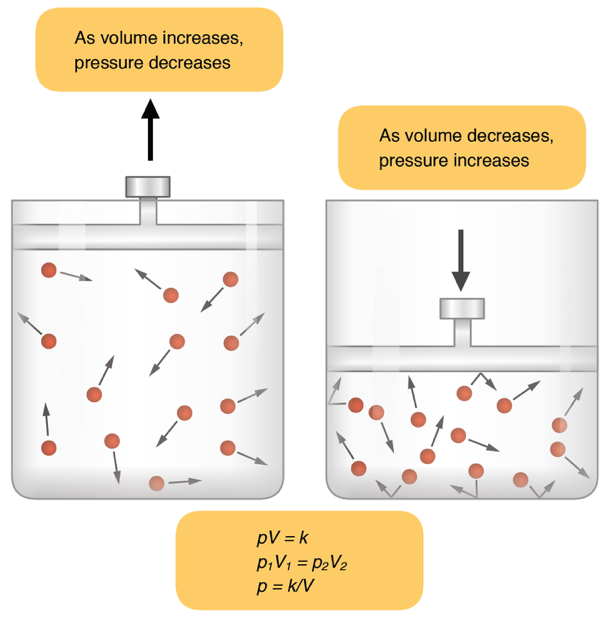
This is true of the body, however the spaces within the body that contain air, including the lungs, sinuses, intestines, and middle ear follow a different law. The gases in these spaces obey Boyle's law; the pressure of a given quantity of gas at constant temperature varies inversely with its volume. Therefore, as you dive deeper, the volume of air in the middle ear, sinuses, lungs, and gastrointestinal tract is reduced. Inability to maintain gas pressure in these body spaces equal to the surrounding water pressure leads to barotrauma.
Boyle’s Law: the pressure of a given quantity of gas at constant temperature varies inversely with its volume.
Source: https://upload.wikimedia.org/wikipedia/commons/2/25/2314_Boyles_Law.jpg
Barotrauma can potentially involve any area with entrapment of gas in a closed space. In addition to sinuses, lungs and the GI tract, the barotrauma can occur to the external auditory canal, includes teeth, the portion of the face under a face mask, and skin trapped under a wrinkle in a dry suit. The tissue damage resulting from such pressure imbalance is commonly referred to as a “squeeze”.
Given that our patient’s only complains were respiratory in nature; hemoptysis, shortness of breath, cough with deep breathing, we will focus on pulmonary barotrauma. Pressure related injury to lung can occur on the way down or as a diver ascends to the surface.
LET’S DIVE DEEPER
Recall from physiology that if you were able to completely exhale, the absolute minimum lung volume remaining is called the residual volume (RV). Lung squeeze occurs when the when the diver descends to a depth at which the total lung volume is reduced to less than the residual volume. At this point, transpulmonic pressure exceeds intraalveolar pressure, causing transudation of fluid or blood from ruptured of pulmonary capillaries. (1) Patients exhibit signs of pulmonary edema and hypoxemia.
Lung Volumes
Source: https://upload.wikimedia.org/wikipedia/commons/8/8c/Vital_Capacity.png
Despite this presumed mechanism of barotrauma of descent, free divers are able to dive to depths beyond those that should cause mechanical damage to the lungs. Other physiologic mechanisms must play a role, although the exact pathophysiology of this condition remains unclear. When diving deep, the chest cavity itself gets smaller and there is central pooling of blood in the chest from the surrounding tissues. The central pooling of blood in the chest equalizes the pressure gradient when the RV is reached and thereby decreases the effective RV. This mechanism increases the pressure in the pulmonary vascular bed causing rupture of the pulmonary capillaries and intrapulmonary hemorrhage. This is the reason that many free divers cough up blood after deep dive. These mechanisms allow the lungs to be compressed down to about 5% of Total Lung Capacity in highly-trained breath-hold champions. (2) Although there are several case reports of lung squeeze occurring with shallow diving, typically with repetitive dives with short surface intervals. (3) An individual’s anatomy, physiologic reserves, underlying pathology and the conditions of the day all play a role in the development of pulmonary barotrauma. (2)
RESURFACING
As a diver ascends, the pressure within the alveoli of the lung increase as the pressure around the diver decreases. Remember Boyle’s law? If intrapulmonary gas is trapped behind a closed glottis, as the diver ascends and the surrounding pressure decreases, the volume of the intrapulmonary gas increases. Increased pressure within the lung causes an increase in transalveolar pressure leading to overexpansion injury and alveolar rupture. (4) A situation of rapid ascent to the surface, such as if a diver runs out of air, panics, or drops his weights, is often the cause of pulmonary barotrauma of ascent. Divers who hold a breath as they ascend and those with obstructive airway diseases, such as asthma or chronic obstructive pulmonary disease, are at increased risk. This was likely the case with our patient, he did not exhale and relieve the building pressure as he ascended, causing his pulmonary barotrauma.
Eventually, the intrapulmonary pressure rises so high that air is forced across the pulmonary capillary membrane. The specific clinical manifestations of pulmonary barotrauma depend on the amount of air that escapes the alveoli and location that it travels to. Air can rupture alveoli, causing localized pulmonary injury and alveolar hemorrhage. (4) Pulmonary interstitial air can dissect along bronchi to the mediastinum causing pneumomediastinum, the most common form of pulmonary barotrauma. This air can track superiorly to the neck, resulting in subcutaneous emphysema. Rarely, air may reach the visceral pleura, causing a pneumothorax.
If air enters the pulmonary vasculature, it can travel to the heart and embolize to other parts of the body, causing arterial gas embolism (AGE). Clinical manifestations of cerebral air embolism are sudden and can be life-threatening. Approximately 4% of divers who suffer an AGE die immediately from Total occlusion of the central vascular bed with air. (5,6) AGE patients who make it to the hospital usually present with hemoconcentration due to plasma extravasation from endothelial injury. (7) The degree of hemoconcentration correlates with the neurologic outcome of the diver. (7) Creatinine kinase is elevated in cases of AGE and correlates with neurologic outcome of the diver. (8) All cases of AGE must be referred for hyperbaric oxygen treatment as rapidly as possible. (9) All suspected AGE patients should be referred for hyperbaric consultation, even if initial neurologic manifestations resolve prior to reaching an ED in order to prevent progression of subtle neurologic deficits that are not immediately detected.
Our patient dove to a depth of 50 feet and reported holding his breath while resurfacing, therefore it is likely that he experienced pulmonary barotrauma of ascent. However, cases of lung squeeze have occurred with free diving to more shallow depths. (3) Regardless, the emergency department management of the spectrum of pulmonary barotrauma is similar.
MANAGEMENT OF PULMONARY BAROTRAUMA
First of all, stop the dive! Ensure the safety of the injured diver and help them relax. Help the injured diver exit the water to prevent any strenuous physical activity. When available, have the diver breath 100% oxygen. Avoid exposure to pressures (such as flying or a repeat dive). On arrival to the ED, perform a complete history and physical. Evaluate for any signs of AGE, such as a transient episode of neurologic dysfunction immediately after surfacing.
A diver with local pulmonary injury without any evidence of AGE does not require recompression and should be treated with supportive care, consisting of rest and supplemental oxygen in severe cases. Most diving-related pneumothoraces are small, therefore treatment may consist simply of supplemental oxygen and close observation. If the diver requires recompression, a chest tube must be placed in order to prevent a tension pneumothorax during depressurization from a hyperbaric chamber. Depending on where you practice, consider transferring the patient to a tertiary care facility if the clinical presentation is worsening, if there are further episodes of hemoptysis, or if the patient requires further testing, such as broncoscopy. To date, I have been unable to find any data that supports the use of steroids, diuretics, or other medications to treat this condition. Patients should rest for at least two weeks before resuming diving and preferably after being cleared fit to dive by a physician with knowledge of dive related injuries.
NEED SOME ADVICE?
Divers Alert Network (DAN) is a not-for-profit diving safety medical organization. DAN's medical staff is on call 24 hours a day, 365 days a year, to handle diving emergencies. They can be reached via DAN.org and through a medical hotline 1-919-684-9111.
TAKE HOME POINTS
Pressure contributes to the majority of diving-related medical problems.
The spaces within the body that contain air, including the lungs, sinuses, intestines, and middle ear obey Boyle's law; the pressure of a given quantity of gas at constant temperature varies inversely with its volume.
As you dive deeper, air in the middle ear, sinuses, lungs, and gastrointestinal tract is reduced in volume. As you resurface, the pressure of the gas decreases and the volume expands.
When breath-hold diving to deep depths, divers may experience “lung squeeze”, or transudation of fluid or blood from ruptured pulmonary capillaries causing non-cardiogenic pulmonary edema.
On ascent, over distension causes alveolar rupture and may cause air to escape into an extraalveolar locations.
Possible presentations are pneumomediastinum, subcutaneous emphysema, pneumothorax, or arterial gas embolization.
Treatment usually consists of supportive care, rest, avoiding further exposure to pressures (flying or repeat dives), and supplemental oxygen when needed.
Evaluate for any historical clues of physical exam findings suggestive of AGE as these patients require hyperbaric treatment.
When in doubt, call the 24-hour Divers Alert Network (DAN) emergency medical hotline at 1-919-684-9111.
Faculty Reviewers: Dr. Kristina McAteer and Dr. Victoria Leytin
Follow the discussion here on Figure 1
SOURCES
Schaefer KE, Allison RD, Dougherty JH, Jr., et al. Pulmonary and circulatory adjustments determining the limits of depths in breathhold diving. Science 1968;162:1020-3.
Lung Squeeze: Coughing your lungs out...or not! 2015. (Accessed July 15, 2018, at https://alertdiver.eu/en_US/articles/lung-squeeze-coughing-your-lungs-out-or-not.)
Raymond LW. Pulmonary barotrauma and related events in divers. Chest 1995;107:1648-52.
Balk M, Goldman JM. Alveolar hemorrhage as a manifestation of pulmonary barotrauma after scuba diving. Ann Emerg Med 1990;19:930-4.
Van Hoesen K., Lang, M. Diving Medicine. Auerbach’s Wilderness Medicine. 7th ed: Elsevier, Inc.; 2017:1583-618.
Neuman TS, Jacoby I, Bove AA. Fatal pulmonary barotrauma due to obstruction of the central circulation with air. J Emerg Med 1998;16:413-7.
Smith RM, Van Hoesen KB, Neuman TS. Arterial gas embolism and hemoconcentration. J Emerg Med 1994;12:147-53.
Smith RM, Neuman TS. Elevation of serum creatine kinase in divers with arterial gas embolization. N Engl J Med 1994;330:19-24.
Cales RH, Humphreys N, Pilmanis AA, Heilig RW. Cardiac arrest from gas embolism in scuba diving. Ann Emerg Med 1981;10:589-92.