Brown Sound: Ultrasound Diagnosis of Ectopic Pregnancy
CASE
A 36 year-old female presented with the acute onset of abdominal pain. She had taken multiple home pregnancy tests, all of which were positive, and then experienced a bout of severe dizziness. On physical exam, she was very pale, and had a tender abdomen. Soon after arrival, the patient became unresponsive. During this episode, the patient became tachycardic, but maintained spontaneous respirations. She was placed in reverse trendelenburg, and multiple attempts were made to get an automated blood pressure reading with no luck. Finally, a manual blood pressure of 70/58 was obtained. Fluid resuscitation was initiated and bedside ultrasound was performed:
Using a curvilinear probe, the ultrasound showed a complex mass with pockets of simple fluid in the suprapubic area. Additionally, free fluid was visualize in Morrison’s pouch (the space between the liver and kidney).
DIAGNOSIS
Ruptured ectopic pregnancy
DISCUSSION
An ectopic pregnancy occurs when an egg implants outside the uterus (extrauterine). Most occur in the Fallopian tube, but they can also occur in the cervix, C-section scars, ovaries, or even the abdomen.[1] An ectopic pregnancy should be considered in any female patient with a positive pregnancy test and abdominal pain and/or vaginal bleeding. When these patients are hypotensive or otherwise unstable, a ruptured ectopic pregnancy should be suspected. In these cases, point-of-care ultrasound (POCUS) can be an incredibly useful, even lifesaving, adjunct.
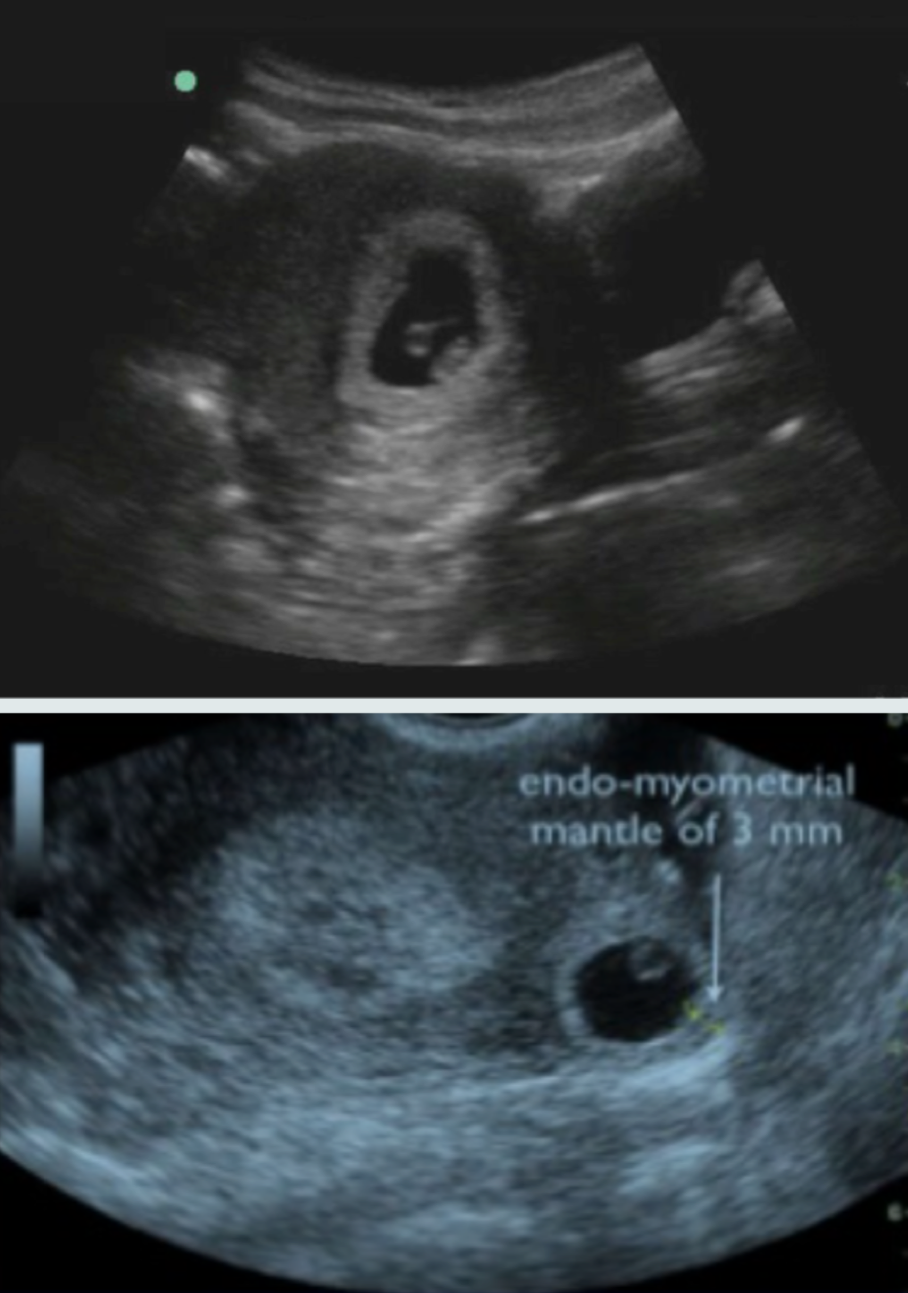
The goals of POCUS are to check for a definitive intrauterine pregnancy (IUP) and to look for intraabdominal free fluid. To effectively rule-out an ectopic pregnancy via ultrasound, an intrauterine pregnancy (IUP) must be visualized.[2] A definitive IUP has a yolk sac or fetal pole in a gestational sac within the uterus (Figures 1 and 2). In very early pregnancy (less than 5 weeks), only a gestational sac will be seen in the uterus.[3] Additionally, the endomyometrial mantle (the edge of gestational sac to edge of myometrium) must be greater than 5 mm (Figure 2). If these structures are not seen in these anatomical positions, an ectopic pregnancy cannot be excluded.
Figure 1. Ultrasound diagnosis of IUP. (Courtesy of Dr. Kristin Dwyer, Director of Ultrasound Division of Brown Emergency Medicine)
Figure 2. Top: Definitive IUP on POCUS. Bottom: Apparent IUP, but with endomyometrial mantle of 3 mm. (Courtesy of Dr. Kristin Dwyer, Director of Ultrasound Division of Brown Emergency Medicine)
If an ectopic pregnancy is suspected, Morrison’s pouch should also be interrogated to evaluate for free fluid. In a study of patients with ectopic pregnancies, 9 out of 10 patients with fluid in Morrison’s pouch ultimately underwent emergent operative intervention.[4]
An important, but rare, consideration is heterotopic pregnancy. Heterotopic pregnancy involves an intrauterine with a concurrent extrauterine pregnancy.[5] This is a very rare occurrence, except among women undergoing in vitro fertilization (IVF). The overall incidence is 1 in 30,000 pregnancies, but increases to 1 in 3,900 with the use of assisted reproduction techniques [5,6]. In these cases, an IUP would be seen on POCUS, but there would be another pregnancy in an another extrauterine location. There must be a high degree of suspicion for heterotopic pregnancies, as they are very difficult to diagnose.
CASE RESOLUTION
A positive pregnancy test, hypotension, and an ultrasound showing a complex pelvic mass with abdominal free fluid (and no definitive IUP) significantly raised the level of suspicion for an ectopic pregnancy in this patient. In the setting of active intraabdominal bleeding, a blood transfusion was initiated and she was taken to the operating room for surgical management.
TAKE HOME POINTS
Ectopic pregnancy should be considered in any female patient with a positive pregnancy test and abdominal pain or vaginal bleeding.
A point-of-care ultrasound should be performed to assess for ectopic pregnancy and free intra-abdominal fluid.
To diagnose an IUP, there must be a yolk sac or fetal pole inside a gestational sac within the uterus, with a myometrial mantal thickness greater than 5 mm.
For further reading on this topic, please check out these previous posts: A Tale of Two Bleeders, Ultrasound Case of the Month (January 2017), and Clinical Image of the Month (September 2018).
FACULTY REVIEWER
Dr. Kristin Dwyer
REFERENCES
Bowyer J, Coste J, Fernandez H, Pouly JL, Job-Spira N. (2002). Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod. 2002; 17(12):3224
Barnhart KT. Ectopic pregnancy. N Engl J Med. 2009; 361:379-387.
Doubilet PM, Benson CB, Bourne T, Blaivas, M. Diagnostic Criteria for Nonviable Pregnancy Early in the First Trimester. Ultrasound Q. 2014; 30(1):3–9.
Moore C et al. Free fluid in Morison's pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007; 8:755-8
Reece EA, Petrie RH, Sirmans MF, Finster M, Todd WD. Combined intrauterine and extrauterine gestations: a review. Am J Obstet Gynecol. 1983; 146(3):323-330.
Tal J, Haddad S, Gordon N, Timor-Tritsch I. Heterotopic pregnancy after ovulation induction and assisted reproductive technologies: a literature review from 1971 to 1993. Fertil Steril. 1996; 66(1):1-12.