Pediatric Magnet Ingestion: When Magnets Stack- Scope it Stat?
CASE
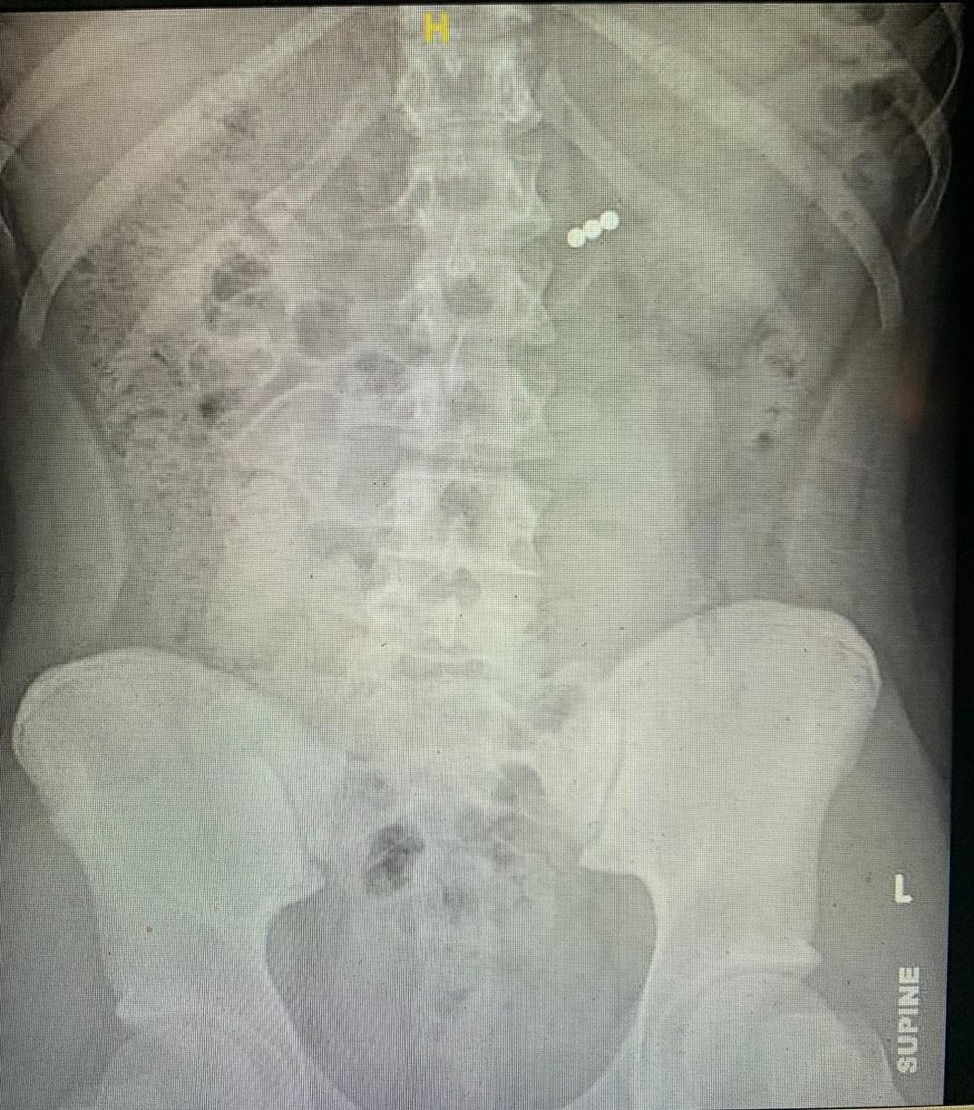
A 12 year old male presents to the ED from an outside hospital (OSH) after accidentally ingesting 3 ‘buckyballs‘ while playing with a toy just prior to arrival. He was building a structure and had them in his mouth when he accidentally swallowed them. He denies any abdominal pain, vomiting, nausea, or other symptoms since ingestion. Image obtained at the OSH demonstrated the following findings and he was transferred to a tertiary care center for further evaluation and care.
Figure 1: Image obtained of 3 buckyball ingestion localized to the stomach area.
DIAGNOSIS
Pediatric Magnet Ingestion
DISCUSSION
Ingestion of foreign bodies is a frequent emergency in the pediatric population and ingested magnets pose a serious health risk to children. This is a growing issue, with 22,000 magnet ingestions reported between 2001-2011. (1) While less than 1% required surgery, those that required intervention had significant morbidity with findings including bowel necrosis and peritonitis. An informal survey of North American Society of Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) members in Spring 2012 regarding magnet ingestion identified significant morbidity in >80 magnet ingestions, which resulted in 39 endoscopies, 26 surgeries, 26 bowel perforations, and 3 bowel resections. (2) Emergency providers should be knowledgeable about the risks of magnet ingestion and should be familiar with the initial approach to assessment and management of these patients.
Figure 2. Neodymium magnets (left) left and Buckyballs (right) are both types of rare earth magnets found in toys and other household products. (3)
Magnets, specifically powerful rare-earth magnets as shown above, are found frequently in toys and other household objects. They may be marketed by names such as ‘buckyballs’, ‘zen magnets’, ‘neocube’, or ‘nanodots’. (3) Such magnets may be be mistaken for candy by younger children or intentionally ingested by older who children may consume them as a dare. These magnets, which are often composed of neodymium or other rare earth components such as iron or boron, are stronger than traditional magnets and can attract one another with significant force. It is estimated that these magnets have 5-10 times increased strength compared to a traditional refrigerator type magnet. (3)
Once ingested, magnets can become lodged in different areas throughout the GI tract. Magnets isolated to the esophagus or the stomach should be promptly removed by a gastroenterologist. (2) If more than one magnet is swallowed, or a magnet is co-ingested with another metallic object and they progress beyond the pylorus, multiple layers of bowel can become trapped between the two objects, ultimately leading to many dangerous downstream complications.
On presentation, patients may be asymptomatic or present with a range of symptoms including abdominal pain, nausea, vomiting, and even fever. When possible a thorough history should be obtained including type of magnet ingested, time of ingestion, and quantity of ingestion. Imaging should be obtained, most typically with an abdominal radiograph (KUB). Pediatric gastroenterology should be consulted if magnets are isolated to the esophagus or stomach, as these may be retrievable on endoscopy. Pediatric surgery should be consulted if ingestion > 12 hours, magnets are beyond the stomach on imaging, or the patient is symptomatic. Unfortunately, radiographic imaging alone is unable to distinguish whether tissue is lodged between two particular magnets, so especially if a patient is symptomatic, one should maintain high clinical suspicion of magnet related injury.
A proposed algorithm for magnet ingestion, from a paper by Hussain et al (2), is outlined below that highlights important considerations including number of magnets ingested, symptoms, and location. Of course, check for institution specific guidelines.
Figure 3 : Proposed approach to the pediatric patient with magnet ingestion (2)
Complications
Complications from magnet ingestion in pediatric patients have been well characterized. While most magnet ingestions will not require surgical intervention, patients have been noted to develop pressure ulcers, obstruction, volvulus, fistulae, bowel perforation, and even death.(1-5)
Disposition
Patients with multiple magnet ingestion will equire admission to a hospital for at least observation, if not intervention, unless the magnets pass on their own. If not undergoing emergent intervention, often polyethylene glycol is added to facilitate passage though there is not any published data yet to support this approach. (2) In the case of single magnet ingestion, patients may be discharged home if a close follow up is available and a plan is made to monitor for passing of magnet. These decisions should be made in conjunction with a pediatric gastroenterologist and/or surgeon. Patients presenting to an outside hospital should be transferred to a tertiary care center if capacity for intervention via GI or pediatric surgery is not readily available.
CASE RESOLUTION
Pediatric surgery and pediatric GI were consulted on this patient. Given the initial image, the concern was that magnets were located in the stomach, therefore the patient underwent EGD. Magnets were not located, and the patient was therefore admitted for serial KUBs and monitoring. Patient remained asymptomatic, was monitored daily, given a bowel regimen with polyethylene glycol and monitored with KUBs every 6 hours. On day 4, due to failure to progress, he underwent colonoscopy and the magnets were successfully retrieved.
TAKE-AWAYS
Most cases of magnet ingestion involve pediatric patients and although many will resolve without intervention it can lead to life-threatening illness.
Obtain a KUB, and count the number of magnets as well as their relative position
Call GI if any magnets in the stomach or esophagus. Call pediatric surgery if below the stomach and multiple magnets ingested.
Consider transfer to a hospital with pediatric specialties if practicing in the community.
Author: Christina Matulis, MD is a 3rd year Emergency Medicine Resident of Brown University
Faculty Reviewer: Kristina McAteer, MD is an Assistant Professor of Emergency Medicine and Clinician Educator at Brown University
Sources
Bauman, et al. Emergency management of the ingested magnet. Pediatric Emergency Care. 2019 35 (8) e141-e144.
Hussain, S., Bousavaros, and Gilger. Management of ingested magnets in childrens. JPGN. 2012 55(3) 239-242.
Mills, W., and Levine, A. So your kid swallowed a little magnet… Emergency Physicians Monthly. Newsletter. April 2015. https://epmonthly.com/article/what-the-buck-did-you-swallow/
Dutta, S. Barzin, A. Multiple magnet ingestion as a source of severe gastrointestinal complications requiring surgical intervention. Arch Pediatr Adolesc Med 2008; 162(2):123-125.
Strickland, M. et al. Case discussions and radiographic illustration of magnet-related injuries in children. J Emerg Med 2020 Jun; 58(6): 902-909.