A Picture Is Worth a Thousand Words: A Case of Meckel’s Diverticulum
THE CASE
A previously healthy four-month-old boy presented to the emergency department with two bloody stools. Earlier in the morning, the mother went to change his diaper and noted a large maroon colored stool which was sticky with red tinged edges. The mother changed his diaper again around noontime and noted another large maroon stool. His mother brought him to the pediatrician’s office. Upon showing a picture of the stools to the pediatrician, the patient was instructed to present to the emergency department.
Figure 1: Maroon colored stool
The child had several other wet diapers in between stools, and mother noted he had been acting like his normal self, and had no other symptoms including no fevers, vomiting, rhinorrhea, or cough. Patient was up-to-date on vaccinations, had no known medical history. He was formula fed without any recent changes, and was born at full term by spontaneous vaginal delivery.
His vital signs were: BP 88/39, HR 154, RR 44, T 99.8
He was pale appearing, interactive, appeared well hydrated with brisk cap refill, had a soft, nontender, nondistended abdomen with no guarding. External rectal exam did not show any fissures, but was significant for a small ring of bright red blood around his anus.
Labs were significant for a Hgb of 7.5, Hct 24.5. A KUB was ordered which showed a nonobstructive nonspecific bowel gas pattern. An abdominal ultrasound was performed which showed no sonographic abnormalities and no visualized intussusception.
Given the large volume of gastrointestinal bleeding and the lack of other cause identified on ultrasound (i.e. intussusception), we discussed our concern for Meckel’s diverticulum with pediatric gastroenterology. They recommended a Meckel’s scan through nuclear medicine.
Figure 2: Annotated Meckel’s diverticulum scan using Tc-99m pertechnetate with green arrows highlighting physiologic uptake of tracer (normally seen in stomach and bladder) and red arrow highlighting persistent focus of abnormal uptake of tracer in the right mid abdomen (consistent with a Meckel’s diverticulum)
Diagnosis
Meckel’s Diverticulum
DISCUSSION
Meckel’s diverticulum is the most common congenital malformation of the gastrointestinal tract. It is caused by the incomplete regression of the vitelline duct and results in a true diverticulum consisting of all three layers of the intestinal wall. The blood supply is derived the from the right vitelline artery which comes from the superior mesenteric artery. There is an increased association of Meckel’s diverticulum in patients with esophageal atresia, imperforate anus, and omphalocele. [4]
We were all likely first introduced to Meckel’s diverticulum through the infamous rule of 2s. They typically are found in 2% of the population, within 2 feet of the ileocecal valve, 2 inches in length, 2 types of heterotopic mucosa, and/or present before the age of 2.
Meckel’s diverticulum clinical presentation ranges from asymptomatic as an incidental finding to dramatic GI bleeding causing hemorrhagic shock. Meckel’s diverticulum presents most commonly as one of three different presentations or combinations. Lower gastrointestinal bleeding from ulceration of the heterotopic gastric mucosa. Intestinal obstruction from either an internal volvulus or intussusception. Local inflammation causing pain either with or without intestinal perforation, mimicking the presentation of appendicitis [1]
Meckel's can sometimes be diagnosed using modalities such as ultrasound, CT, or MRI, but the sensitivity and specificity of these are low. Symptomatic Meckel’s are more likely to be lined by heterotopic mucosa, most commonly gastric mucosa but can also include pancreatic and colonic tissue. [4] Asymptomatic Meckel’s are more likely to be lined with normal intestinal epithelium. [4] Therefore, nuclear medicine scans with Tc-99m pertechnetate can visualize a Meckel’s diverticulum as the tracer accumulates in the ectopic gastric tissue. A systematic review looking at 562 scans found the sensitivity to be 89.6% with a specificity of 97.1%. [1]
There are several physiologic factors which influence the result of this test. First, a true positive relies on the presence of functional ectopic gastric mucosa within a Meckel’s. If a Meckel’s diverticulum is composed of non-gastric mucosal tissue (i.e. colonic, pancreatic) there may be a false negative result as Tc-99m pertechnetate is not taken up by these tissues. Bleeding can cause extravasation of the tracer contributing to potential false positive and false negative results. Additionally, a Meckel’s may be hidden behind another structure which physiologically accumulates tracer such as the stomach and the bladder. [1]
CASE CONTINUED
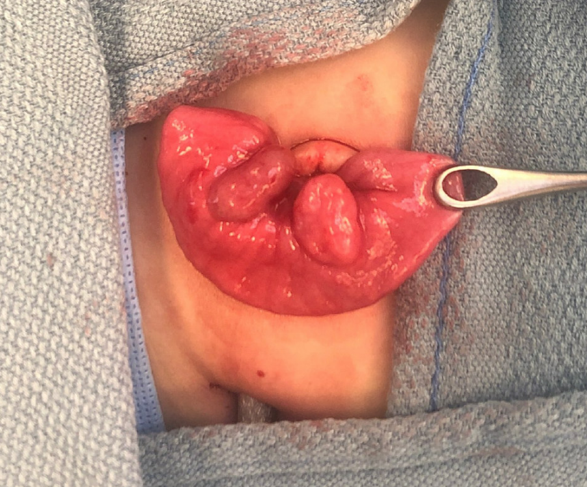
During his time in the emergency department, the patient became more tachycardic with heart rates into the 190s with blood pressures staying in the 80s/30s. He was transfused 20 cc/kg of packed red blood cells resulting in an improvement in his heart rate. Pediatric surgery was consulted, and the patient was taken to the operating room for a diagnostic laparoscopy which identified two areas concerning for Meckel’s diverticulum 3 cm apart from each other in the ileum.
Figure 3: Section of ileum with two intestinal outpouchings taken intraoperatively
A 5cm small bowel resection was performed containing both intestinal outpouchings. The patient did very well post operatively, had return of bowel function on hospital day 2, and was discharged on hospital day 3.
After hospital discharge, the pathology report came back describing two distinct cystic lesions. One was a cystically dilated diverticulum lined by gastric oxyntic-type epithelium, consistent with a Meckel’s diverticulum. The other was a cystic lesion with no luminal communication, consistent with an intestinal duplication cyst.
WHAT IS A DUPLICATION CYST?
A duplication cyst is a rare gastrointestinal tract malformation which are present in children and adults and they can occur in the ileum, esophagus, and colon. They are often identified on endoscopy, and endoscopic ultrasound can help distinguish them from other gastrointestinal lesions. [2] If symptomatic, duplication cysts are usually resected as they can result in infection, obstruction, hemorrhage and/or ulceration. There have been case reports of duplication cysts converting into malignancy. If asymptomatic, there is some debate as to whether surveillance with intermittent endoscopy versus early elective resection is the best treatment in order to prevent some of the above complications. [2]
Interestingly, both ileal intestinal duplication cysts and Meckel’s diverticulum can present with GI bleeding. So, for our patient, what caused the bleed? It is hard to say. Both pathology specimens contained hemorrhage. Nonetheless, both were resected, and the patient did very well post operatively and had no further bleeding episodes.
take-aways
Remember the rule of 2s for
Typical presentations include lower GI bleeding, intestinal obstruction, or with pain episodes and peritonitis similar to appendicitis.
The sensitivity and specificity for Meckel’s diverticula on ultrasound, CT, or MRI is relatively low
Nuclear medicine scans with Tc-99m pertechnetate are very specific and more sensitive than other studies.
AUTHOR: Dr. Brendan Innes is a second-year emergency medicine resident at Brown University/Rhode Island Hospital
FACULTY REVIEWERS: Dr. Meaghan Beucher is an Assistant Professor of Pediatric Emergency Medicine and Clinician Educator at Brown University/Hasbro Children’s Hospital.
Dr. Don Yoo is Director of Nuclear Medicine at Miriam Hospital and Professor of Diagnostic Imaging and Clinician Educator at Brown University
REFERENCES
Hansen C-C, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Medicine (Baltimore). 2018;97(35). doi:10.1097/MD.0000000000012154
Liu R, Adler DG. Duplication cysts: Diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound. 2014;3(3):152-160. doi:10.4103/2303-9027.138783
Sagar J, Kumar V, Shah DK. Meckel’s diverticulum: a systematic review. J R Soc Med. 2006;99(10):501-505.
Stallion A, Shuck JM. Meckel’s Diverticulum. Surgical Treatment: Evidence-Based and Problem-Oriented. Zuckschwerdt; 2001. Accessed April 21, 2021. https://www.ncbi.nlm.nih.gov/books/NBK6918/