Fire-related Injuries in Children
It is a typical busy pediatric shift at the tertiary care center. You receive advanced notification that a pediatric code is in progress after a child was extricated from a house fire, now approximately five minutes out. How will you set up the room? Who do you need to notify? What resources are at your disposal?
With this frightening scenario in mind, the need for an intimate understanding of both the trauma protocols and pediatric burn therapy becomes clear.
DISCUSSION
As in any patient with a traumatic presentation, the first order of business is the primary survey. When following ATLS guidelines, providers are expected to correct each problem in the order in which it is evaluated before moving onto the next. [1] In the following sections, additional considerations for burns and inhalation injury are included.
Primary Survey, with specific considerations for burn/inhalation injuries [2,3]
In general follow the alphabet A, B, C, D and E. The first and most important part of the primary survey is Airway. A provider should have a low threshold to intubate if there are signs of: significant respiratory distress, airway edema, facial burns, burns in the mouth, singed facial hair, large burns who may need large amounts of fluid resuscitation, or a decreased level of consciousness.
Next assess the patient’s Breathing – if inhalation injury is suspected, start the patient on 100% high flow oxygen while preparing for airway protection. Check Circulation (blood pressure, IV access, hemorrhage, pulses) and assess for circumferential burns as they can impair blood flow. Start fluid resuscitation early (prehospital or on arrival) as described in later paragraphs.
Then assess for Disability, signs of altered mental status, or consideration for other trauma. Lastly a provider must obtain Exposure and Environmental control. First stop the burning process – remove clothing, jewelry, diapers etc. and rapidly assess for other major injuries. Keep the patient warm because children do not regulate temperature as well.
Secondary Survey, with specific considerations for burn/inhalation injuries [2,3]
The standard secondary survey includes repeat and tertiary exams as well as advanced history gathering. Pay attention to whether the burn occurred inside or outside, and whether there was smoke exposure. When possible, ask whether any fuel or other chemicals were present as well as about any other trauma (ex. jump out window, blast injury).
Complete a full head to toe exam, and obtain a pertinent medical history, allergies, etc. As discussed further in later paragraphs, calculate total body surface area of any burns (TBSA) and use this calculation to plan for rate of resuscitation.
Burn Classification
Burns were traditionally classified as 1st, 2nd, or 3rd degree, however more recently this system has been replaced by one reflecting the need for surgical intervention. This classification system includes superficial, superficial partial-thickness, deep partial-thickness, and full-thickness. Deep burns involve the fascia/muscle. [4]
Cutaneous burn classification. UpToDate. UpToDate, Inc.; 2021. https://www.uptodate.com/contents/image?imageKey=SURG%2F73309&topicKey=SURG%2F819&search=burn&rank=2~150&source=see_link.
Extent of the Burn
It is important to calculate the extent of the burn in terms of total body surface area (TBSA), as this value is used in the calculation for fluid resuscitation. Also keep in mind that it can take 48-72 hours for the full extent and depth of the burn to be determined. Only 2nd and 3rd degree burns are included in the calculation of TBSA. [2,3,6 ]
Rule of 9s is another method of estimation (quick and easy, but less accurate).
Medzcool. The Rule of Nines. Nucleotype. https://www.nucleotype.com/rule-of-nines/. January 4, 2020. Accessed March 29, 2021. https://www.nucleotype.com/rule-of-nines/
The following diagram is for children ≤1 year old. However providers should know that these diagrams/percentages change as child gets older – as age increases, head percentage decreases and leg percentage increases which makes the rule of 9s less useful in pediatrics.
Medzcool. The Rule of Nines. Nucleotype. https://www.nucleotype.com/rule-of-nines/. January 4, 2020. Accessed March 29, 2021. https://www.nucleotype.com/rule-of-nines/
Palm Rule is a simple rule for burn size estimation in both children and adults with small surface area burns. The extent of the burn can be measured using the size of the patient’s entire hand (palm plus fingers) as 1% and adding up the burned areas. [2,6]
Stiles K (2018) Emergency management of burns: part 2.
Lastly Lund-Browder is another more detailed method used by burn centers for burn estimation. [2,3]
Children are not small adults.
There are many differences between children and adults that have significant impact in burn management. In burn care, children 14 and older are treated as adults. Important considerations in younger children include [2,3]:
Airway:
Airway is narrower than adults, therefore less edema is needed to obstruct airway (lower threshold to intubate if inhalation injury suspected)
Larynx more anterior
Glottis is more angulated and more anterior
Narrowest portion of airway in children is cricoid cartilage (vs glottis in adults)
Tongue is proportionally larger
Epiglottis is larger and floppier.
Thinner skin: Children typically have thinner skin. This predisposes them to deeper burns compared to adults exposed to similar temperatures and exposure durations. [2]
Temperature regulation: Children have an impaired ability to maintain their core temperature, so they are at greater risk for hypothermia (core temperature <95°F). Hypothermia can lead to deeper burns as it causes vasoconstriction.
Body Surface Area: Children have a different distribution of body surface area. This must be taken into account when calculating TBSA for fluid resuscitation. In general, children have larger heads and smaller legs for the purpose of TBSA calculations. [2]
Fluid resuscitation: Children have a greater surface area per unit body mass than adults. This means that they require larger amounts of resuscitation fluids than adults. Additionally, children have a smaller intravascular volume per surface area/unit body mass and are therefore more susceptible to over-resuscitation. [2,3]
Glucose/Maintenance Fluids: Young children (≤30kg) and infants require maintenance fluids with dextrose as they have limited glycogen stores and can easily become hypoglycemic. [2,3]
Fluid Resuscitation
In patients with burn injuries, fluid resuscitation is one of the most important aspects of treatment. Burns cause cytokine release which leads to increased vascular permeability and vasodilation which leads to fluid loss and hypotension. Fluid resuscitation aims to counteract this by supporting organ perfusion. [2] The preferred choice of fluid for resuscitation is Lactated Ringers (LR). [2,3]
Ideally, fluids will be started pre-hospital or immediately upon arrival. Until TBSA can be calculated during the secondary survey, fluids should be started at the following recommended rates. [2]
Once the TBSA is calculated, the following calculations can be used. Traditional teaching states that the total amount of fluids for 24 hours is divided with the first half being given over 8 hours and the second half being given over the next 16 hours. However, in practice this is rarely the case. Instead, the calculations are used to get an initial rate, and once fluids are started they are titrated to the patient’s urine output. [2,3]
Additionally, as mentioned above, young children and infants have limited glycogen stores and require maintenance fluids with dextrose in addition to standard burn resuscitation fluids. In infants and children ≤30kg, add D5LR at maintenance rate. [2,3] A helpful pediatric rule for maintenance fluids is to give 4ml/kg/hr for the 1st 10kg, 2ml/kg/hr for the 2nd 10kg, and 1ml/kg/hr for any remaining kg over 20kg. So for example a 12 kg toddler would receive 44mL per hour and a 25 kg child would receive 65 ml per hour.
Other Important Considerations
Circumferential Burns: Can occur on extremities and around the chest and abdomen. Important considerations for circumferential burns of the extremities are continued pulse checks and keeping the limb elevated to reduce swelling. Circumferential burns can also occur around the chest and abdomen. Circumferential burns in the chest are particularly problematic for children as they have more pliable rib cages, and therefore must work harder to breathe and expand the chest against constriction caused by the circumferential burn. The treatment for circumferential burns is an escharotomy. [2,3]
Heat loss: All patients should be kept warm with clean, dry sheets. This is especially important in young children who cannot easily regulate their temperatures as well as adults. [2]
Infection and Tetanus: All burn patients should receive a tetanus shot if they are not up to date. While infection is a major risk for burn patients, prophylactic antibiotics are not recommended. [2]
Labs: In addition to standard labs (CBC, BMP, glucose, etc) and EKG, an ABG, carboxyhemoglobin level and cyanide level are recommended for all patients with fire exposure and possible smoke inhalation.[2,3] Approximately 30% of pediatric patients with burns have concomitant inhalation injuries as described below in special considerations. [7]
Special Considerations
Carbon Monoxide
Carbon monoxide (CO) is an odorless, tasteless gas that is created by incomplete combustion. CO binds to hemoglobin with an affinity 200 times greater than oxygen, therefore displacing oxygen from hemoglobin. Hemoglobin that binds to CO is called carboxyhemoglobin. When hemoglobin can no longer carry a sufficient amount of oxygen, tissue hypoxia occurs. [2,8]
Symptoms of CO poisoning vary depending on the level of CO. [8] Levels of 5-10%, often found in smokers and people living in heavy pollution areas are typically asymptomatic. Levels of 15-40% can cause headache, blurry vision, nausea, and vomiting. Whereas levels greater than 40% can bring about confusion, seizure, coma and death.
Typically the patient’s pulse oximetry reading will be normal as the pulse oximeter is unable to differentiate between carboxyhemoglobin and oxyhemoglobin. Previously the only way to measure the amount of CO was to obtain a carboxyhemoglobin level. More recently, a co-oximeter can be used as it is able to differentiate between carboxy- and oxy-hemoglobin and can give a more accurate reading. [2,8]
When checking labs, typically the blood gas analysis with be normal, other than the carboxyhemoglobin level.
Treatment for CO poisoning consists of 100% oxygen and potentially hyperbaric oxygen. Patients presenting from a house fire with any concerning symptoms, even a mild headache, should raise suspicion for CO poisoning and immediately be placed on 100% O2 which works by decreasing the half-life of CO from 4 hours to 1 hour. In severe cases, hyperbaric oxygen can also be considered. These include cases where CO levels are > 25%, there is loss of consciousness or altered mental status, severe metabolic acidosis, or concern for end-organ damage. [2,8]
Hydrogen Cyanide
The second toxin produced from fires is cyanide, which comes from the combustion of synthetic products, including carpet, plastics, upholstery, vinyl, and wool. [2,9]
Cyanide creates toxicity by entering cells and binding and inhibiting mitochondrial cytochrome oxidase, an important complex in the electron transport chain. This inhibition in turn halts oxidative phosphorylation and the production of ATP via the Krebs cycle (aerobic pathway). Cells then shift towards anaerobic metabolism, causing lactic acidosis. [9,10]
Bridwell R. EM@3AM: Cyanide Toxicity. emDOCs.net. July 17, 2020. Accessed March 29, 2021. http://www.emdocs.net/em3am-cyanide-toxicity/
It is thought that children are more susceptible to cyanide poisoning. They have higher respiratory rates, resulting in increased inhalation. Additionally, they have lower body mass and immature metabolism result in higher toxicity for smaller amounts of cyanide than adults. [10]
Symptoms of cyanide poisoning are similar to those of CO poisoning, including headache, confusion, seizures, and coma. It also causes irritations of the eyes and mucous membranes. [9] As CO begins to affect the cardiovascular system, there is a hyperdynamic phase (tachycardia and hypertension) followed by circulatory collapse (hypotension and bradycardia). [10] Traditionally, cyanide produces a “bitter almond” odor, though not everyone can detect the scent and it is not a sensitive finding. [9]
While cyanide levels can be measured, it is typically not a rapid test and treatment needs to be started prior to obtaining the actual level. One diagnostic clue to cyanide poisoning, especially in fire victims who are at high risk, include metabolic acidosis with persistently elevated lactate (>8). [9]
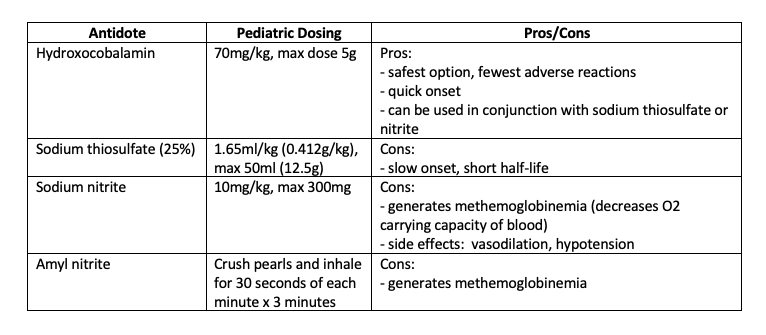
When cyanide poisoning is suspected, patients should be treated empirically. Hydroxocobalamin is the antidote of choice given its tolerability and very few adverse reactions. [9,10] Cyanide has a higher affinity for cobalt than cytochrome oxidase resulting in the formation of cyanocobalamin (vitamin B12), which is nontoxic and easily excreted in the urine. [9] Other medications include sodium thiosulfate, sodium nitrite, and amyl nitrite (the old cyanide kits included all three). Nitrites work by oxidizing hemoglobin to methemoglobin, which complexes with cyanide to form nontoxic cyanomethemoglobin. [10] Typically, 20-30% methemoglobin is necessary to bind cyanide, but these levels can be fatal in children. Therefore, nitrites are typically not recommended for children. [10] Symptomatic treatment includes IV fluids and vasopressors for hypotension and benzodiazepines for seizures.
Criteria for Transfer
The American Burn Association recommends that pediatric burn patients be transferred to a Burn Center in the following situations [2,3]: infants and children with any full thickness burn, burns to face, hand, feet, genitalia or perineum, Partial thickness burns if >10% TBSA or with any full thickness component, or if hospital does not have qualified personnel or equipment for care of children.
TAKE AWAY POINTS
Start fluid resuscitation pre-hospital or during primary survey
5 years and younger: 125ml LR/hr
6-13 years: 250ml LR/hr
14 years and older: 500ml LR/hr
Estimate burn surface area using the palm rule (palm + fingers = 1%, add up burned areas)
Important differences in pediatric patients
Airway anatomy -> low threshold to intubate
Thinner skin -> deeper burns
Impaired temperature regulation
Different body surface area distribution in pediatrics impacts fluid resuscitation calculations, don’t over resuscitate.
Young children require additional glucose-containing fluids
Patients exposure to fire and smoke likely have a component of carbon monoxide and cyanide poisoning and providers should treat empirically if high suspicion or significant exposure.
CO poisoning is treated with 100% oxygen
Cyanide poisoning is treated with Hydroxocobalamin
AUTHOR: Stephanie Hess, MD
FACULTY REVIEWER: Meghan Beucher, MD
References
American College of Surgeons Committee on Trauma. Advanced Trauma Life Support (ATLS) Student Course Manual, 10th ed, American College of Surgeons, Chicago, IL; 2018.
American Burn Life Support Advisory Committee. Advanced Burn Life Support Course Provider Manual 2018 Update. American Burn Association, Chicago, IL; 2018.
Sheridan, RL. Chapter 375: Thermal Injuries. In: McInerny TK, Adam HM, Campbell DE, DeWitt TG, Foy JM, Kamat DM, eds. American Academy of Pediatrics Textbook of Pediatric Care. 2nd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2017.
Mertens DM, Jenkins ME, Warden GD. Outpatient burn management. Nurs Clin North Am. 1997; 32:343.
Cutaneous burn classification. UpToDate. UpToDate, Inc.; 2021. https://www.uptodate.com/contents/image?imageKey=SURG%2F73309&topicKey=SURG%2F819&search=burn&rank=2~150&source=see_link
Medzcool. The Rule of Nines. Nucleotype. https://www.nucleotype.com/rule-of-nines/. January 4, 2020. Accessed March 29, 2021. https://www.nucleotype.com/rule-of-nines/
Barrow RE, Spies M, Barrow LN, Herndon DN. Influence of demographics and inhalation injury on burn mortality in children. Burns. 2004;30(1):72-77. doi:10.1016/j.burns.2003.07.003
Sen S. Pediatric inhalation injury. Burns Trauma. 2017;5:31. doi:10.1186/s41038-017-0097-5
Bridwell R. EM@3AM: Cyanide Toxicity. emDOCs.net. July 17, 2020. Accessed March 29, 2021. http://www.emdocs.net/em3am-cyanide-toxicity/
Mintegi S, Clerigue N, Tipo V, et al. Pediatric cyanide poisoning by fire smoke inhalation: a European expert consensus. Toxicology Surveillance System of the Intoxications Working Group of the Spanish Society of Paediatric Emergencies. Pediatr Emerg Care. 2013;29(11):1234-1240. doi:10.1097/PEC.0b013e3182aa4ee1