Lymphadenopathy in Pediatric Population
INTRODUCTION
The goal of this post is to give you a systematic approach to a pediatric patient with lymphadenopathy. The differential is broad and the etiology ranges from benign to life threatening, and is most commonly benign. As such, to be a successful emergency room practitioner, it is vital to have a defined approach and know when to tune into high risk features.
CASE
A 12-year-old boy with no significant medical history presented to the emergency department due to an abnormal lymph node. The patient had a primary care appointment several days prior. His PCP felt a large left inguinal lymph node. The patient was sent for an outpatient ultrasound to further evaluate this lymph node.
The ultrasound results were as follows:
“2.3 cm left para-aortic node.
3.7 x 1.1 x 3.1 cm anterior mesenteric node at the level the umbilicus
1.7 x 0.5 x 0.8 cm right lower quadrant lymph node
1.3 cm right inguinal node
2.9 x 1.3 x 2.5 cm left inguinal node
2.3 x 0.9 x 1.7 cm left inguinal node
3.4 x 1.5 x 1.9 cm left internal iliac node
2.4 x 1.6 x 2.4 cm left internal iliac node”
The patient denied any associated symptoms. No fevers, no chills, no nausea, no vomiting, no recent travel history. This patient was sent to the emergency department for immediate evaluation of the results. His physical exam is notable for a 3-4 cm by 2 cm left inguinal node that is slightly firm, nontender, and mobile. No other pertinent findings.
BACKGROUND
A lymph node is a small bean-shaped structure. It is an important part of the body’s immune system. A lymph nodes’ role is to filter substances that travel through the lymphatic fluid. Lymph nodes contain lymphocytes that help the body fight infection and disease. There are hundreds of lymph nodes throughout the body [1]. They are connected to each other by lymphatic vessels.
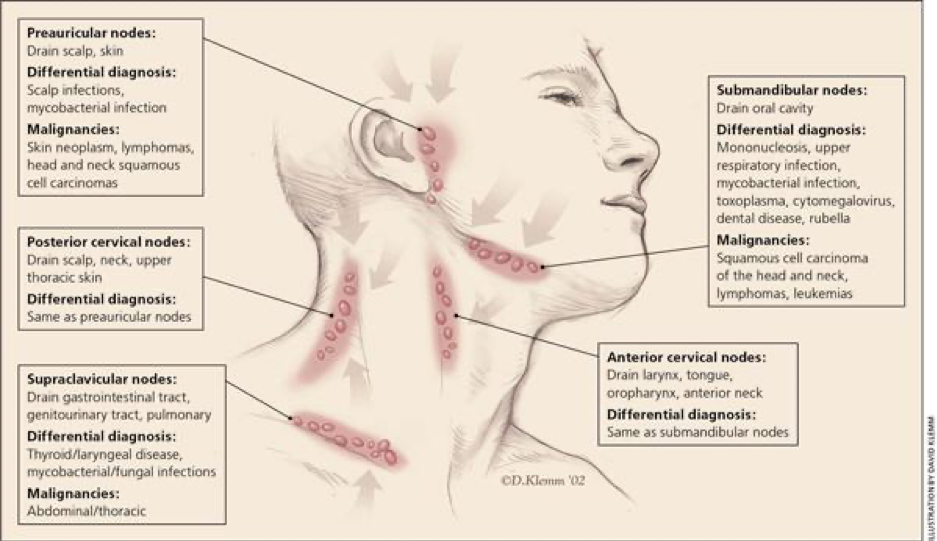
Bazemore AW, Smucker DR. Lymphadenopathy and malignancy. Am Fam Physician. 2002;66(11):2106.
Bazemore AW, Smucker DR. Lymphadenopathy and malignancy. Am Fam Physician. 2002;66(11):2106.
Figure 1. Classification of lymph nodes
Bazemore AW, Smucker DR. Lymphadenopathy and malignancy. Am Fam Physician. 2002;66(11):2106.
There are many ways to further classify lymph nodes. Below are a few important categories that you can use:
Duration: How long has it been present? [3]
Acute lymphadenopathy: lasts up to two weeks
Subacute lymphadenopathy: lasts for 4-6 weeks
Chronic lymphadenopathy: lasts >6 weeks
Size: What is too big? [4]
Lymph nodes greater than 1 cm are abnormal (although sizing varies based on anatomic location)
Any palpable supraclavicular, popliteal, and iliac nodes are considered abnormal
Epitrochlear nodes > 5 mm are abnormal
Abdominal lymph nodes >10 mm are abnormal
Retrocrural lymph nodes> 6 mm are abnormal
Retroperitoneal lymph nodes> 10 mm are abnormal
Pelvic lymph nodes >8-10 mm are abnormal
Looking back at the ultrasound that was performed on our patient, there are various lymph nodes that were abnormal based solely on size (highlighted below).
“2.3 cm left para-aortic node.
3.7 x 1.1 x 3.1 cm anterior mesenteric node at the level the umbilicus
1.7 x 0.5 x 0.8 cm right lower quadrant lymph node
1.3 cm right inguinal node
2.9 x 1.3 x 2.5 cm left inguinal node
2.3 x 0.9 x 1.7 cm left inguinal node
3.4 x 1.5 x 1.9 cm left internal iliac node
2.4 x 1.6 x 2.4 cm left internal iliac node”
Granulomatous versus non-granulomatous [5]
Examples of granulomatous lymph nodes include the below subcategories
● Infectious
○ Suppurative
■ Example: tularemia, yersinia, cat-scratch, lymphogranuloma
○ Non-suppurative
■ Tuberculous, atypical mycobacteria, toxoplasmosis, syphilis
● Non-infectious
○ Sarcoidosis
○ berylliosis
Localized vs Generalized lymphadenopathy
We can also classify lymphadenopathy as localized or generalized. Localized refers to a specific lymph node region. Generalized lymphadenopathy, defined as two or more involved regions, often indicates underlying systemic disease [2]. There are benign and malignant causes that could cause generalized lymphadenopathy. Benign causes include self-limited viral illnesses, such as infectious mononucleosis or medications. Risk factors for malignancy include age older than 40 years, male sex, white race, supraclavicular location of the nodes, and presence of systemic symptoms such as fever, night sweats, and unexplained weight loss. Concerning etiologies to generalized lymphadenopathy include acute HIV infection, activated mycobacterial infection, cryptococcus, cytomegalovirus, Kaposi sarcoma, and systemic lupus erythematosus. Generalized lymphadenopathy can also occur with leukemias, lymphomas, and advanced metastatic carcinomas.
Red flag symptoms for lymphadenopathy include arthralgias, muscle weakness, rash, fever, chills, fatigue, and malaise.
Differential diagnosis for lymphadenopathy can be remembered with the MIAMI mnemonic [2]:
M: malignancies
I: infections
A: autoimmune disorders
M: miscellaneous or unusual conditions
I: Iatrogenic causes
https://www.aafp.org/afp/2016/1201/hi-res/afp20161201p896-t1.gif
In most cases, the history and the physical examination alone can identify the cause of lymphadenopathy. For example, symptoms such as fever, night sweats, weight loss or node located in the supraclavicular, popliteal, or iliac region, bruising, splenomegaly should clue a clinician into diagnoses such as leukemia, lymphoma, solid tumor metastasis. With patients who have high-risk sexual behavior, clinicians should think about chancroid, HIV, lymphogranuloma venereum, and syphilis. Patients who have fever, chills, malaise, sore throat, without other red flag symptoms, you should consider pathology such as bacterial or viral pharyngitis, hepatitis, influenza, mononucleosis, and rubella.
For pediatric patients, about one half of otherwise healthy children have palpable lymph nodes at any one time. Lymphadenopathy lasting less than two weeks or greater than 12 months without change in size has low likelihood of being neoplastic. Exceptions to this rule include low-grade Hodgkin lymphomas and indolent non-Hodgkin lymphoma.
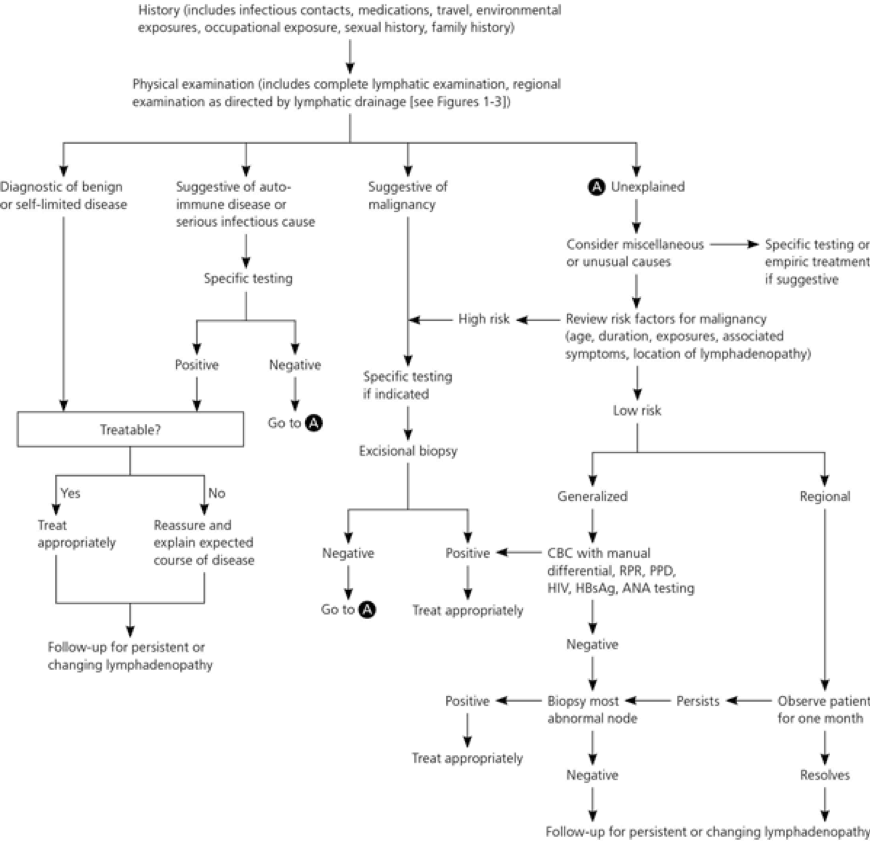
Workup for a patient with lymphadenopathy [2]:
The American College of Radiology recommends ultrasonography as the initial imaging choice for cervical lymphadenopathy in children up to 14 years of age and computed tomography for persons older than 14 years [6].
CASE RESOLUTION
To summarize, we have a 12 year old boy who is completely asymptomatic and found to have left inguinal lymphadenopathy. He had an outpatient ultrasound which prompted an emergency department visit. In the emergency department, the patient had broad laboratory workup including CBC, CMP, EBV, LDH, Uric Acid, ESR, CRP, Lipase, EBV, CMV, Bartonella, and germ cell tumor markers (AFB, HCG). All of which were within normal limits or negative. Patient also had a CT chest, abdomen, pelvis to better define abdominal lymphadenopathy as well as to assess lymphadenopathy above the diaphragm. CT imaging showed: Enlarged lymph nodes noted along the left iliac chain and periaortic region as noted on recent ultrasound. No enlarged lymph nodes are identified superior to the diaphragm. As before, histologic sampling is recommended. Patient was referred to pediatric hematology oncology and pediatric surgery for further evaluation and decision whether or not a biopsy is indicated. At this time, the patient has been lost to follow up with outpatient providers.
AUTHOR: Anita Knopov, MD is a current third year emergency medicine resident at Brown University/Rhode Island Hospital.
FACULTY REVIEWER: Meghan Beucher, MD
References:
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/lymph-node
https://www.aafp.org/afp/2016/1201/p896.html#afp20161201p896-b15
https://pubmed.ncbi.nlm.nih.gov/22706525/
American College of Radiology. ACR Appropriateness Criteria: neck mass/adenopathy. https://acsearch.acr.org/docs/69504/Narrative/. Accessed December 1, 2016.