Unresolved UTI: The Search For a Prompt Diagnosis
CASE
A 14-year-old female presented to the emergency department (ED) with persistent left upper quadrant (LUQ) pain. She was last seen in the ED one week prior for similar symptoms. Initially, she was diagnosed with a urinary tract infection (UTI), treated with IV ceftriaxone, and discharged home on a course of cefdinir. On re-presentation, she complained of persistent LUQ pain, fevers with a Tmax of 103 F, and one episode of emesis overnight. Physical examination revealed abdominal tenderness in the LUQ, without ipsilateral CVA tenderness.
The care team was concerned about potential upper urinary tract complications given the prolonged symptoms coupled with high fevers in the setting of adequate antimicrobial coverage. Our differential included acute pyelonephritis (APN), perinephric abscess, or acute obstruction. The choice was made to do a bedside renal and bladder ultrasound followed by a comprehensive ultrasound. The following obtained images showed both a decrease in vascular flow and a pronounced wedged-shaped echogenicity in the pole of the left kidney (Figures 1 and 2).
Figure 1: Left kidney on bedside ultrasound.
Figure 2: Left Kidney on comprehensive ultrasound.
DIAGNOSIS
Given the ultrasound findings consistent with known signs of APN coupled with a urine analysis consistent with a bacterial infection she was diagnosed with APN. She was started on IV antibiotics and admitted to the hospital for further treatment. No CT imaging was obtained throughout her hospital course. She was discharged home on hospital day two and has not had a recurrent UTI.
DISCUSSION
UTIs are common in children and young adolescents, with an estimated range of 6-8% in older children with urinary symptoms. This age group has a bimodal distribution, with a higher incidence in infants/toddlers and older adolescents [4]. We divide infections involving the urinary tract into upper and lower tract infections. These etiologies can commonly be distinguished using a thorough history and physical exam. Classically upper UTI will present with abdominal pain with systemic features including fever, anorexia, nausea, vomiting, lethargy, and malaise. In contrast, lower UTIs will present with lower abdominal pain or suprapubic pain, dysuria, urinary frequency, and urgency [4].
For most patients with suspected acute complicated UTI the use of imaging is unwarranted except in the patients who are severely ill, have persistent clinical symptoms despite 48 to 72 hours of appropriate antimicrobial therapy, or have suspected urinary tract obstruction [4]. The use of a point of care ultrasound (POCUS) exam for assistance with a diagnosis of pyelonephritis is not yet standard of care in the emergency department. The most common finding on ultrasound in a patient with APN is a benign POCUS exam [3,8]. However, there are specific classic lesions that one can visualize on ultrasound. These include loss of corticomedullary differentiation, increased size of the kidney, loss of renal sinus fat due to edema, a dilated renal pelvis, and urothelial thickening [7]. In this case, we visualized a wedge-shaped and linear pattern of echogenicity in the renal parenchyma with a loss of blood flow to these areas [7].
Figure 3. Acute pyelonephritis, Power doppler image with grayscale in a 24-year-old woman shows the characteristic echogenic striated appearance of the kidney with distinct wedge-shaped areas of increased parenchymal echogenicity and associated hypoperfusion. CT imaging on the right for comparison [7].
CT is still the more commonly used imaging modality when there is a clinical need for a definitive diagnosis. As CT allows for the identification of gas, hemorrhage, obstruction, or stones more precisely than ultrasound [7]. However, CT increases radiation and ties up additional resources in the emergency department.
However, recent research and improved ultrasound technology may be changing our clinical accuracy with diagnosing upper UTI pathology. A recent retrospective study shows that 39.6% of ED patients demonstrated significant abnormalities associated with upper UTIs, including hydronephrosis, renal abscess, and emphysematous pyelonephritis [1]. This percentage increased to 60.9% in complicated cases. Additionally, roughly 33% of patients had findings that diverted the patient directly to surgical intervention for percutaneous nephrostomy, abscess aspiration, ureteroscopic stone manipulation, lithotripsy, or nephrectomy. Thus in these cases POCUS had a profound change in the trajectory of their hospital course. A follow up study looked at the effectiveness of ultrasound vs. CT vs. MRI to detect APN [3]. The results showed that 25.6% of patients demonstrate a pronominal renal pyramid sign on POCUS [3]. This is increased echogenicity of the kidneys except for the region of renal pyramids and is a finding consistent with our patient outlined above. Although these papers show the rate at which known lesions linked with upper UTI etiologies are identified using POCUS, they fail to provide data on the sensitivity or specificity of POCUS. Currently, the diagnostic sensitivity and specificity of POCUS techniques are far less than a CT image. One recent study demonstrated a sensitivity of only 33.3% using ultrasound versus 81.0% using CT for discovering upper UTI etiologies [7]. Therefore, although some signs can be useful to the bedside clinician that may prompt further desire to seek a CT, thus far no study has shown ultrasound alone should be enough to rule in or out a case of acute complicated UTIs.
However, newer technology in ultrasound just on the horizon shows great promise in potentially changing this current state. Superb microvascular imaging aims to visualize low velocity and small-diameter blood vessel flow. This process shows promise in characterizing liver lesions, breast masses, and thyroid nodules. A recent study sought to compare Microvascular Doppler US to conventional Doppler US [2]. This retrospective study included 28 adolescent children with 41 known APN lesions as characterized on CT or DMSA. Of these lesions, 52.8% were visible on B-mode, 85.4% on conventional color Doppler US, and 94.3% on microvascular ultrasound. Although the inter-observer agreement was only moderate, there is potential as practitioners gain more access to the microvascular US for it to increase our ability to determine and characterize upper UTI pathologies including APN.
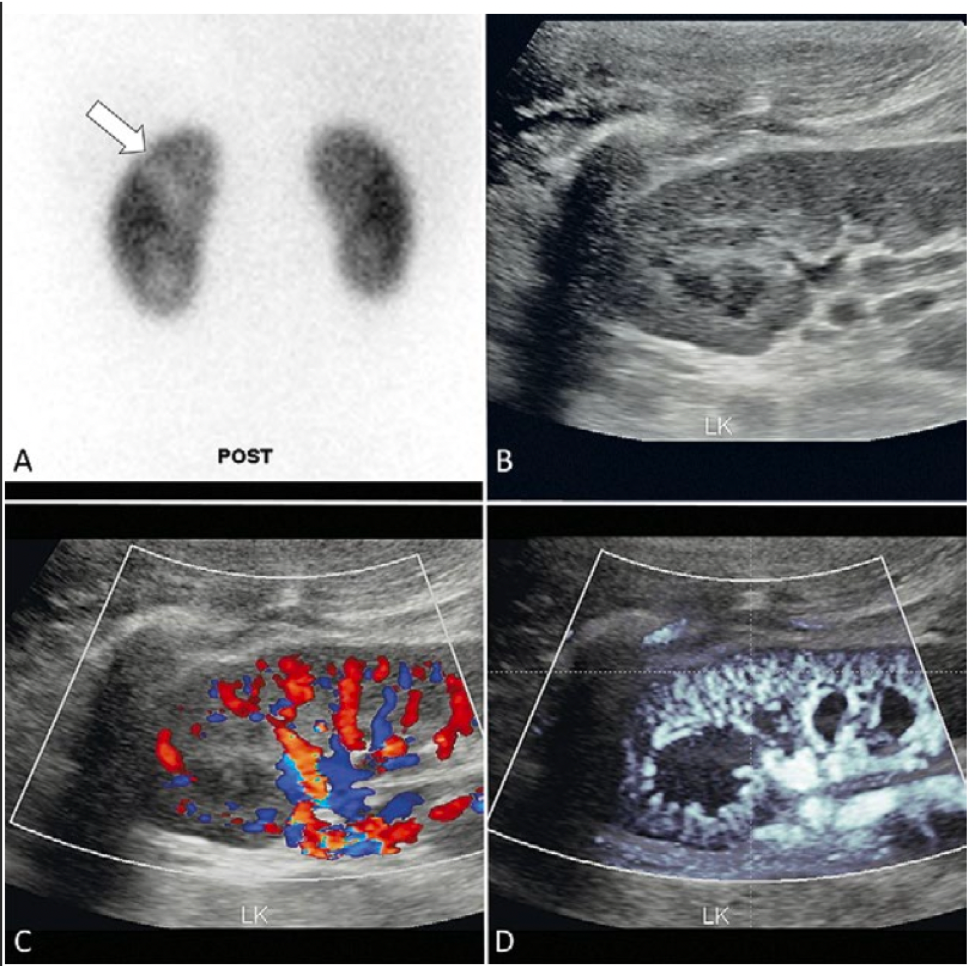
Figure 4. A 12-year-old girl with febrile UTI. (A) DMSA scan confirmed APN in the upper (arrow) and lower poles of the left kidney. B-mode (B), color Doppler (C), and microvascular Doppler (D) for the upper pole lesion. All three readers interpreted an APN lesion on C and D, but not B. All of them reported that the lesion distinguishability and diagnostic confidence between C and D were equal [2].
TAKE-AWAYS
Most cases of acute complicated UTIs do not require advanced imaging. The exception is when certain key clinical features are present. These include patients who are severely ill, have persistent clinical symptoms despite 48 to 72 hours of appropriate antimicrobial therapy or have suspected urinary tract obstruction.
Currently, CT imaging is the standard for definitive characterization of these acute complicated UTIs both in the ED and in the inpatient setting.
If present, key findings on POCUS can lead to a more definitive diagnosis that can change the course of a patient's hospital admission.
Emerging ultrasound technology has the potential to allow clinicians to obtain more detailed information about upper UTI etiologies perhaps one day supplanting the need for CT imaging.
AUTHOR: Brian Drury, MD is a first-year emergency medicine resident at Brown University/Rhode Island Hospital.
FACULTY REVIEWER: Kristin Dwyer, MD MPH is an Assistant Professor of Emergency Medicine at Brown Emergency Medicine and Emergency Ultrasound Fellowship Director
References
Chen, K. C., Hung, S. W., Seow, V. K., Chong, C. F., Wang, T. L., Li, Y. C., & Chang, H. (2011). The role of emergency ultrasound for evaluating acute pyelonephritis in the ED. Am J Emerg Med, 29(7), 721-724. https://doi.org/10.1016/j.ajem.2010.01.047
Choi, G., Je, B. K., Hong, D., & Cha, J. (2021). Microvascular Doppler ultrasound in children with acute pyelonephritis. Med Ultrasound, 23(2), 161-167. https://doi.org/10.11152/mu-2827
Enikeev, D. V., Glybochko, P., Alyaev, Y., Enikeev, M., & Rapoport, L. (2017). Imaging technologies in the diagnosis and treatment of acute pyelonephritis. Urologia, 84(3), 179-184. https://doi.org/10.5301/uj.5000234
Hooton, T., Gupta, M. Acute Complicated urinary tract infection (including pyelonephritis) in adults. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (Accessed on November, 1, 2021.)
Kaufman, J., Temple-Smith, M., & Sanci, L. (2019). Urinary tract infections in children: an overview of diagnosis and management. BMJ Paediatr Open, 3(1), e000487. https://doi.org/10.1136/bmjpo-2019-000487
Simıes E Silva, A. C., Oliveira, E. A., & Mak, R. H. (2020). Urinary tract infection in pediatrics: an overview. J Pediatrian (Rio J), 96 Suppl 1, 65-79. https://doi.org/10.1016/j.jped.2019.10.006
Vourganti, S., Agarwal, P. K., Bodner, D. R., & Dogra, V. S. (2006). Ultrasonographic evaluation of renal infections. Radiol Clin North Am, 44(6), 763-775. https://doi.org/10.1016/j.rcl.2006.10.001
Yoo, J. M., Koth, J. S., Han, C. H., Lee, S. L., Ha, U. S., Kang, S. H., … & Lee, Y.S. (2012). Diagnosing acute pyelonephritis with CT, 99m Tc-DSMA SPECT, and Doppler ultrasound: A comparative study. Korean journal of urology, 51(4), 260-265
Zulfiqar, M., Ubilla, C. V., Nicola, R., & Menias, C. O. (2020). Imaging of Renal Infections and Inflammatory Disease. Radiol Clin North Am, 58(5), 909-923. https://doi.org/10.1016/j.rcl.2020.05.004