The assessment of extraocular movement (EOM) and pupillary light reflex can be used to evaluate for ocular injury post-trauma. However, many patients with ocular trauma can present with significant orbital edema or pain that limits assessment due to the physician being unable to retract the eyelids. Ocular ultrasound provides a unique way to assess the eyes in the event of a trauma without causing significant pain or harm to the patient. This blog post provides techniques on how to perform ocular ultrasound to assess EOM and pupillary light reflex…
Read MoreBy: Russell Prichard MD and Melanie Lippman MD
CASE
The patient is a 52 year-old female with a past medical history of hypertension, hyperlipidemia, hypothyroidism, and a 2 pack a day smoking history who presented to the emergency department in respiratory distress.
When EMS arrived to the patient’s home, she was hypoxemic with a pulse oximetry reading of 70s on room air and hypotensive with systolic blood pressures in the 80s. She was placed on nasal cannula with improvement in her saturations and she was given aspirin, fentanyl, and nitroglycerin without relief.
Upon arrival her vitals were significant for respiratory rate of 34, pulse oximetry of 98% on 6L NC. She was noted to be in acute distress.
The patient was placed on positive pressure ventilation via BiPAP and broad blood work, chest X-ray and electrocardiogram (ECG) were obtained.
Read MoreAn otherwise healthy 6 year-old female presented with lower abdominal pain and non-bloody, non-bilious emesis since 11:00 PM the previous night. Several hours prior to the onset of her symptoms, she was playfully thrown into a pond where she was swimming. She subsequently had take-out brown rice and vegetables with her family. Nobody else developed symptoms. Her pain was worse with ambulation and bumps in the road. She has had no diarrhea, constipation, fevers, urinary symptoms, or other acute complaints. She had similar but less severe episodes of these symptoms in the past. The patient’s father had a history of a “blood disorder” requiring abdominal surgery…
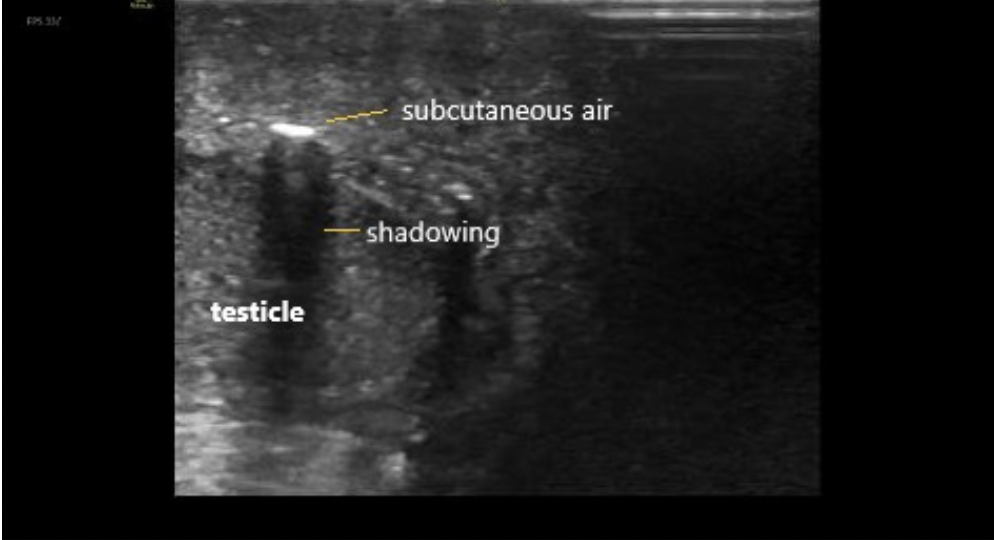
Read MoreA 60 year-old male with history of poorly controlled diabetes, congestive heart failure, chronic kidney disease, and a prior MI presented as a transfer from an outside hospital for surgical management of suspected necrotizing fasciitis/Fournier’s gangrene. He reported symptoms of diarrhea, nausea, vomiting, and severe pain in the scrotum and perineum for several days. This began after he sustained a small cut to the area. He denied fevers, urinary discharge, respiratory symptoms, chest pain, but did endorse chills and night sweats…
Read MoreWhen a patient presents to the emergency department with atraumatic monoarticular arthritis, it is important to rapidly determine the etiology because septic arthritis is a medical emergency that can lead to significant morbidity and mortality…
Read More