Not so Funny Bone - Traumatic Arthrotomy of the Elbow
“A TAE occurs when a lesion extends into the joint capsule of the elbow, contaminating the articular space of a joint and increasing risk of infection. Patients typically present to the ED as a trauma (such as an motor vehicle collision or gunshot wound). Early identification of TAEs allows for…”
What is a traumatic arthrotomy of the elbow (TAE)?
A TAE occurs when a lesion extends into the joint capsule of the elbow, contaminating the articular space of a joint and increasing risk of infection. Patients typically present to the ED as a trauma (such as an motor vehicle collision or gunshot wound). Early identification of TAEs allows for timely washout and debridement. Inadequately identified and managed TAEs increase patients’ risks of septic arthritis, decreased mobility, chronic pain, and mortality [1].
When should I suspect a TAE?
Any deep lesion near the elbow! Especially if it is leaking synovial fluid, or has air bubbles or fat droplets. X-rays may suggest TAEs if there is intra-articular free air, a foreign body, or a fracture [2]. However, x-rays without these findings are not sufficient to rule out a TAE [3].
What is the approach to TAE detection?
Traumatic arthrotomies are generally identified with a saline load test or a CT scan. Unlike traumatic arthrotomies of the knee, where several studies have supported the use of CT as a validated method of detection [4], this evidence is particularly lacking for the elbow. Two recent studies reported detection of TAE with 100% sensitivity via CT in cadavers. However, more robust data and clinical trials will be required to inform standard of care [5,6]. While research in this area continues, literature recommends that the saline load test should remain the go-to test for TAE evaluation [7].
Saline load test technique:
Of note, this is a painful procedure and may require procedural sedation. At minimum, consider IV pain medication.
Gather: Sterile saline, lidocaine, chlorhexidine, 50cc syringe, 10cc syringe, 18g needle, 25g needle
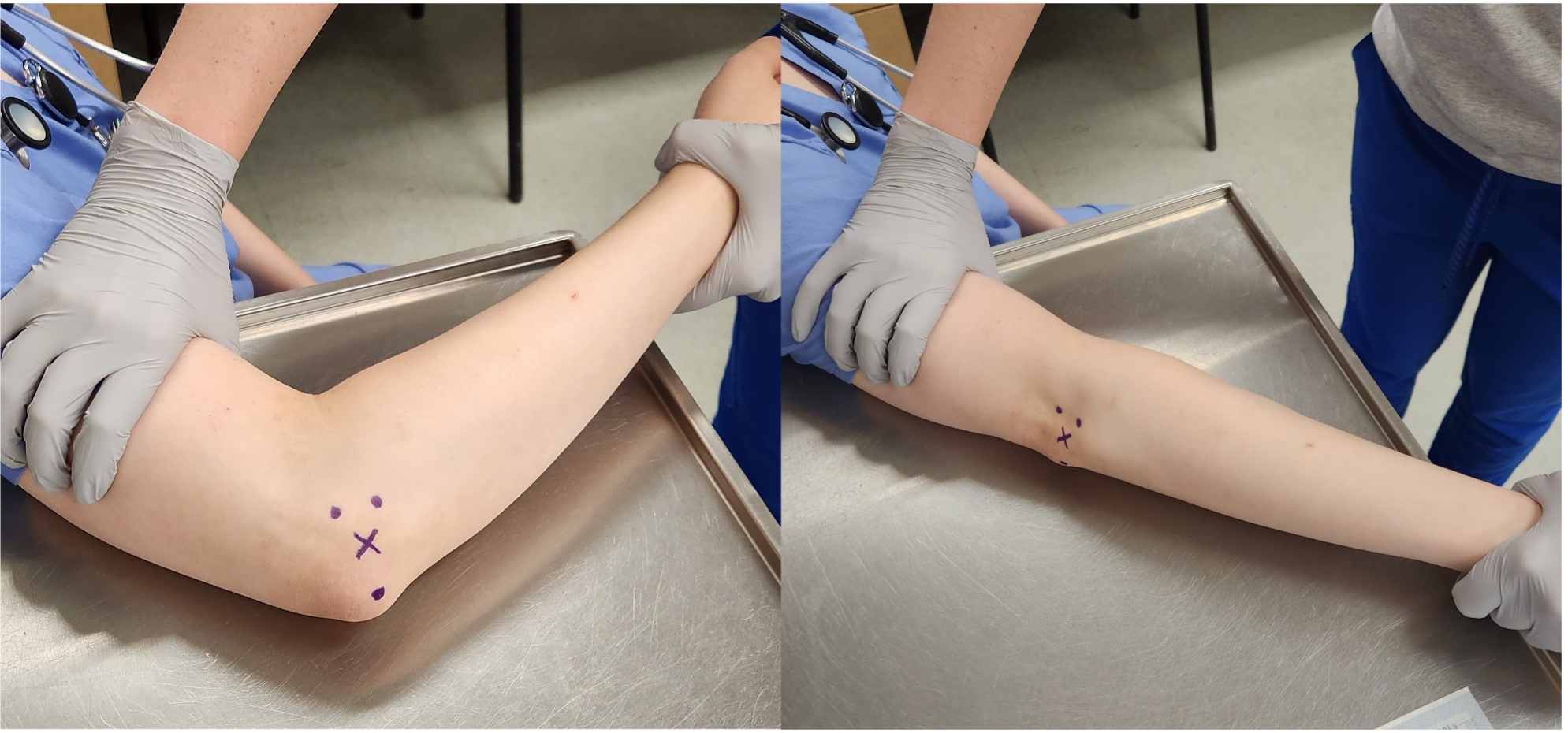
2. Place the patient's elbow in 90 degrees of flexion, in a prone position. Identify the soft spot between the olecranon, lateral epicondyle, and radial head. This is where you will inject (if the lesion is over this area, consider injecting from another location). Sterilize the area with chlorhexidine.
3. Create a wheal and numb the tract with lidocaine
4. Using the 18g needle, aspirate as you advance until you aspirate synovial fluid. This indicates that you are in the joint space. Inject lidocaine to anesthetize the joint space, then inject between 20-40cc of sterile saline and evaluate for fluid leaking out of the injury site (which indicates a positive test). Range the elbow from 90 to 180 degrees and evaluate for a fluid leak. The recommended injected quantity of sterild saline varies in literature. Consider starting with 20cc, then slowly adding 2cc at a time until you have a positive test result or until you reach 40cc, as tolerated by the patient. While 20cc has been shown to have a 72% sensitivity for detection of TAEs, ranging the elbow will increase the sensitivity to 86%. At 40cc, the sensitivity increases to 95% [8]. A recent study suggests that at least 26cc with intermittent ranging is recommended to rule out TAEs [9].
5. Remove the injected saline at the end of the test (ideally equivalent to the amount injected if the test was negative)
Now what?
If the saline load test is positive, call orthopedic surgery for washout and debridement. Reduce any fractures, irrigate the lesion, and splint the elbow. Assure the patient is appropriately vaccinated against tetanus. Start antibiotics based on the mechanism and extent of injury. Cefazolin is generally a good choice for injuries with minimal soft tissue damage and without soil or water contamination. Extend coverage with ceftriaxone and metronidazole if there is extensive soft tissue damage and contamination. Remember to cover for Vibrio with piperacillin-tazobactam and doxycycline if there is seawater exposure. Finally, remember to adequately manage the patient's pain.
TAKE-AWAYS
If not detected in a timely manner, TAEs are high risk for poor outcomes (i.e. septic arthritis, mortality, etc).
Suspect a TAE with deep lesions near the elbow, x-ray findings of periarticular air/foreign bodies/fracture, or synovial fluid/fat droplets leaking from the site of injury.
A saline load test is the preferred method of TAE evaluation. Use 20-40cc of saline with ranging the joint to increase sensitivity of detection (at least 26cc with intermittent ranging is recommended to rule out a TAE).
CT is not a validated measure for evaluating TAEs (but be on the lookout for upcoming research in this area).
AUTHOR: Aquilla Chase, MD, MS, is a first year resident at Brown University Emergency Medicine
FACULTY REVIEWERl Kristina McAteer, MD, is an attending physician and Rhode Island Hospital and Newport Hospital