The Pediatric Respiratory Score
Case:
A 3-year-old presents to the ED with shortness of breath. She was feeling well at preschool that day, but at pick-up her mom noted some wheezing. She received a breathing treatment at home that did not help, so she was brought into the ED to be evaluated. You take a quick look at the vitals before going into the room:
RR: 20/min
O2 Sat: 95%
HR: 134
BP: 101/64
Temp: 98.5
You walk into the room and see a 3-year-old girl sitting still on her mom’s lap, leaning forward. You note that she is breathing about 50 times per minute, has intercostal retractions, and inspiratory and expiratory wheezing. You give her three duonebs and dexamethasone, and check on her in 20 minutes. This new exam shows:
RR: 40/min
Expiratory wheezing
Intercostal retractions|
Short bursts of activity followed by coughing
She has no appetite despite not eating in the past 6 hours
You see that she is getting better, and place an order for a few more albuterol treatments while you decide what to do next. Should she be admitted? Floor or PICU? Your hospital just opened up an observation unit for patients like this. But should you expect that she’s going to be able to go home in 24 hours?
Lucky for you, there are many tools available to assess respiratory status, decrease ED length of stay, and try to predict need for admission of children with asthma exacerbation. You decide to use the Pediatric Respiratory Score developed at Seattle Children’s Hospital in 2004.
What is the evidence behind the PRS score?
The PRS score was developed as an intuitive expert opinion-based score that was internally validated to be easy to use by multiple providers (MDs, RNs, RTs). The score was later shown to decrease ED LOS at that institution, but did not decrease inpatient or PICU admissions, or inpatient LOS (Rutman 2016). In November of 2016, Hasbro Children’s Hospital adopted this scoring system as a triage tool for its Pediatric Clinical Decision Unit.
How do you use it?
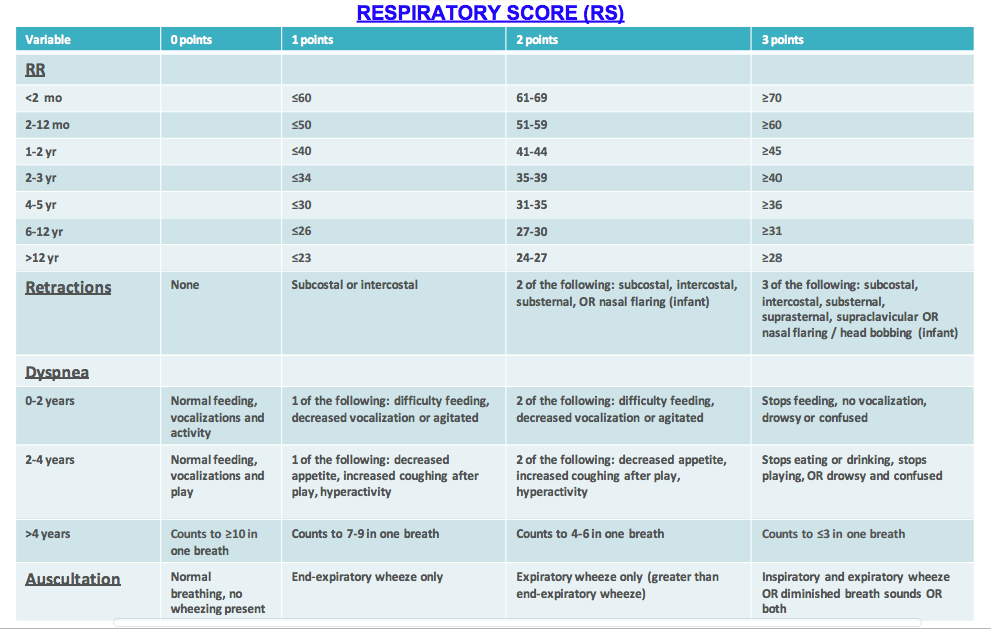
The score is made up of four categories that are evaluated with a score of 0-3. While the table is large, most of it is composed of specific respiratory rate cut-offs. It is designed to be user friendly, but not something to commit to memory.
Figure 1: Respiratory Severity Score
The number calculated from this table is then used to determine further care after the initial round of therapy is administered in the ED (Albuterol +/- ipratropium x 3 and dexamethasone or other corticosteroid).
Treatment options:
Albuterol: Beta-2 agonist that causes bronchodilation. 0.15mg/kg/dose every 20-30 minutes, maximum doses and frequency determined by side effects. Meta-analyses have not shown metered dose inhalers (MDI) to be superior or inferior to nebulized medication (Cates 2013). Nebulizers require less active participation of the patient, and allow for coadministration of ipratropium, but up to 90% of the medication is lost into the air (Rubilar 2000). This loss of medication, though, does not appear to affect efficacy. When using MDIs, it is reasonable to give up to 8 puffs/dose depending upon weight (4 puffs for 5-10kg, 6 puffs for 10-20kg, 8 puffs >20kg), though there are many dosing strategies that are effective (NHLBI 2007), so your institution may have different protocols.
Ipratropium: Anticholinergic, bronchodilator that works through smooth muscle relaxation. 250mcg/dose for children <20kg, 500mcg/dose for children >20kg. It has been shown in RCTs and meta-analyses to decrease admission and improve lung function for severe exacerbations. (Griffiths 2013).
Magnesium: 25-75mg/kg (with a dose max of 2g) over 30 minutes. It was shown in one meta-analysis to decrease admission when combined with albuterol, ipratropium, and steroids (Rubilar 2000).
Steroids: Help to decrease inflammation associated with asthma exacerbation, and are shown to decrease relapse admissions. Prednisone and dexamethasone are of similar efficacy, though dexamethasone can be hard to dose orally since it is only available in pill form (though crushing and masking with yogurt are options). However, prednisone is associated with more vomiting and requires more doses than dexamethasone’s (5-10 vs 1-2) (Cronin 2016).
Terbutaline: A parenteral beta-2 agonist, sometimes given subcutaneously intramuscularly, or intravenously (not FDA approved for IV) for severe asthmatics who cannot cooperate with nebulizers (NHLBI 2007).
Case Conclusion:
This exam would give the pediatric patient an 8 on the PRS pathway, so you decide to transfer her to the observation unit for further evaluation and treatment. She is continued on albuterol every two hours, has continued improvement in her respiratory status over the next 12 hours, and is able to be discharged home in the morning.
Resources:
Seattle Children’s Asthma Pathway: www.seattlechildrens.org/pdf/asthma-algorithm.pdf
Figure 2: Hasbro Children’s Asthma Pathway
Hasbro Children’s Exclusion Criteria (will need intranet connection): https://remote.lifespan.org/pediem/documents/,DanaInfo=intra.lifespan.org+HasbroPCDUAdmissionGuideline.pdf
Faculty Reviewer: Dr. Chris Merritt
References:
Sangrador CO, González de Dios J. “Management of acute bronchiolitis in emergency wards in Spain: variability and appropriateness analysis (aBREVIADo Project).” European Journal of Pediatrics. 171(7):1109-19.
Cates CJ, Welsh EJ, Rowe BH. “Holding chambers (spacers) versus nebulisers for beta-agonist treatment of acute asthma.” Cochrane Database Syst Rev 2013.
Cronin JJ, McCoy S, Kennedy U, et al. “A Randomized Trial of Single-Dose Oral Dexamethasone Versus Multidose Prednisolone for Acute Exacerbations of Asthma in Children Who Attend the Emergency Department.” Ann Emerg Med 2016; 67:593.
Griffiths B, Ducharme FM. “Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children.” Cochrane Database Syst Rev 2013.
Scarfone R. “Acute asthma exacerbations in children: Emergency department management.” Uptodate. 22 June 2016.
Rutman, L., Migita, R., Spencer, S., Kaplan, R., Klein, E. J., & Walthall, J. “Standardized Asthma Admission Criteria Reduce Length of Stay in a Pediatric Emergency Department.” Academic Emergency Medicine, 23(3), 289–296. 13 Feb 2016.
Rubilar L, Castro-Rodriguez JA, Girardi G. “Randomized trial of salbutamol via metered-dose inhaler with spacer versus nebulizer for acute wheezing in children less than 2 years of age.” Pediatr Pulmonol 2000; 29:264.
Rowe BH, Bretzlaff JA, Bourdon C, et al. “Magnesium sulfate for treating exacerbations of acute asthma in the emergency department.” Cochrane Database Syst Rev 2000.
“National Asthma Education and Prevention Program: Expert panel report III: Guidelines for the diagnosis and management of asthma.” (NIH publication no. 08-4051). Bethesda, MD: National Heart, Lung, and Blood Institute, 2007.