EKG Case Report
CASE
A 57-year-old man presents to the emergency department in the middle of the night complaining of chest pain that woke him up three hours ago. He states that he feels tightness and a burning sensation across both sides of his chest, with intermittent sharp pains that he rates as an 8/10. He also reports that both of his arms are numb and tingling, and the right side of his face has been twitching. He has not been able to go back to sleep because he is so uncomfortable.
He has been suffering from GERD for the past month, which has been so severe over the past few days that it has been interfering with his ability to work. The burning sensation that he is now feeling is somewhat similar, but the GERD was never this severe and was not accompanied by the sensory symptoms.
Other than that, he has no known medical problems other than hyperthyroidism for which he does not take any medication. He has a 15 pack-year smoking history, but receives regular medical care and has never been diagnosed with any metabolic diseases. His family history is significant for a brother who had heart problems throughout his life and died of complications at age 49.
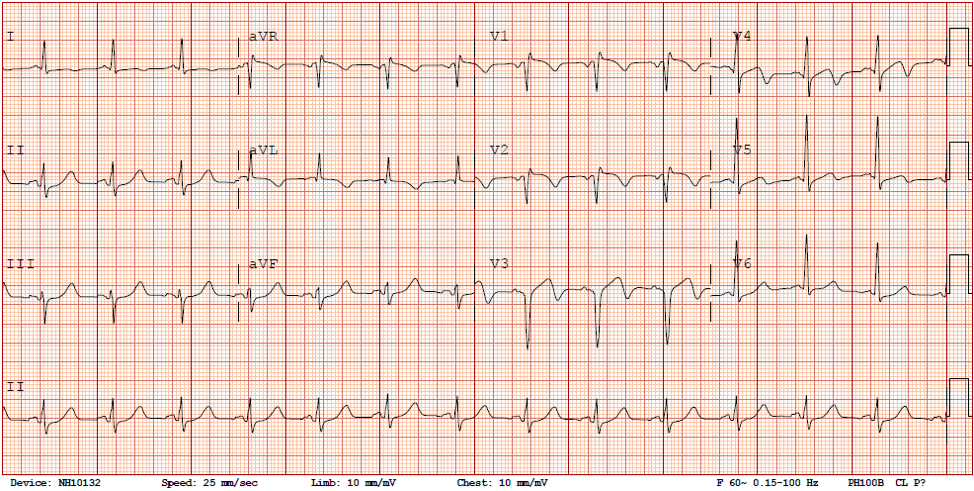
On review of systems, he endorses only chest pain and denies any fever, chills, palpitations, dyspnea, syncope, nausea or vomiting. His blood pressure is elevated at 146/81, but other vital signs and physical exam are normal. His EKG upon arrival to the ED is shown below:
Normal sinus rhythm with a heart rate of 82. The axis is normal as well as the intervals. There are no clear ST elevations but there are biphasic T-waves noted in leads V3, V4, and V5.
ASSESSMENT
57 yo male smoker w/ PMH of GERD presents with three hours of 8/10 substernal chest pain and pressure. This presentation along with his EKG changes and family history of cardiac death are suggestive of ACS. Other potential diagnoses include GERD, esophagitis, or less likely PE or pulmonary pathology.
DIFFERENTIAL DIAGNOSES
Wellens Syndrome:
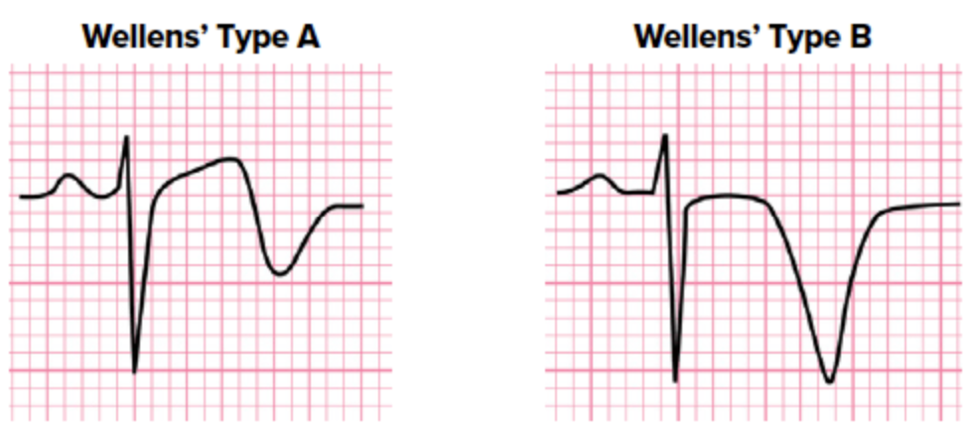
Wellens’ syndrome, or “LAD coronary T-wave syndrome”, describes the EKG changes that are seen in a patient with a critical proximal LAD stenosis. The pathophysiology is believed to involve transient occlusion of the vessel with spontaneous reperfusion. Type A, which occurs earlier in the disease process, involves biphasic T-waves in the precordial leads and type B, which is more common and occurs later, involves deeply inverted T-waves.
Other diagnostic criteria include:
Minimally or non-elevated ST segment
No precordial Q-waves
Preserved precordial R-wave progression
Normal or minimally elevated troponins
Onset of hours to days
These patients have a high likelihood of developing an anterior MI and should be admitted for urgent cardiac catheterization.
STEMI/NSTEMI:
STEMI and NSTEMI both describe conditions where patients present with signs of myocardial ischemia and have elevated troponin levels. They are distinguished based on EKG characteristics, and this classification will determine early management of the patient.
Non-ST elevation myocardial infarction (NSTEMI) is caused by a mismatch between myocardial oxygen demand and blood flow but is not necessarily caused by complete occlusion by a coronary plaque rupture. Other flow-limiting conditions, including stable plaques or coronary vasospasm, can result in NSTEMI.
On EKG, this can manifest with ST depressions +/- T-wave inversions, but without ST elevations or pathologic Q waves. These changes can be diffuse but are often localized to the areas of ischemia. Some possible EKG morphologies include the following:
ST elevation myocardial infarction (STEMI) also involves cardiac ischemia, but is typically a result of transmural ischemia from an obstructive thrombus. On EKG, there initially is J-point elevation with a concave ST segment. Over time, the ST segment becomes more elevated and may even be rounded upward. The criteria for STEMI diagnosis include:
New ST elevation at the J point and two contiguous leads (> 1 mm in any leads other than V2-V3)
In V2-V3, > 1.5 mm elevation in women, > 2 mm in men under 40, or > 2.5 mm in men 40 or older
Among EKGs meeting these criteria, appearance can vary widely and may be similar to any of the following:
CASE RESOLUTION
When the patient was reassessed an hour later, he was resting comfortably but his pain was still a 5/10. He was given another nitroglycerin and a second EKG was obtained. It was relatively unchanged from his initial EKG, with biphasic T waves in V3 and V4 but without any ST elevations > 2 mm. Around this time, his CXR and labs all came back normal except for a troponin of 1.86. Cardiology was called and the patient received heparin while waiting to be transferred for cardiac catheterization.
Emergent angiography showed LAD/diagonal disease with severely elevated LVEDP and EF of 35%. A repeat EKG upon arrival to the tertiary care center showed “ST elevations in the anterior leads with evolving and biphasic T waves”. The patient was diagnosed with an anterior STEMI and two drug-eluting stents were placed in the LAD and Diag1.
The patient had no recurrent chest pain or symptoms of heart failure. He will continue dual antiplatelet therapy (aspirin and prasugrel), statin therapy, a low-dose beta blocker, and lisinopril. Follow-up was recommended with cardiology and cardiac rehab and patient was advised smoking cessation.
AUTHOR: Kathleen Barry is a second year medical student at The Warren Alpert Medical School of Brown University.
FACULTY REVIEWER: Kristina McAteer, MD is Assistant Professor of Emergency Medicine at Brown University.
REFERENCES
Cadogan, M. (2020). Life in the Fast Lane. Wellens’ Syndrome. https://litfl.com/wellens-syndrome-ecg-library/.
ECG and Echo Learning. Clinical ECG Interpretation. https://ecgwaves.com/topic/brugada-syndrome-ecg-treatment-type-1-2-3/.
Basit H, Malik A, Huecker MR. Non ST Segment Elevation Myocardial Infarction. [Updated 2020 Oct 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513228/
Akbar H., Foth C., Kahloon R.A., et al. Acute ST Elevation Myocardial Infarction. [Updated 2020 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532281/
Reeder, G., Kennedy, H. (2020). UpToDate. Diagnosis of acute myocardial infarction. https://www.uptodate.com/contents/diagnosis-of-acute-myocardial-infarction?search=diagnosis%20ami&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
Simons, M., Alpert, J. (2020). UpToDate. Acute coronary syndrome: Terminology and classification. https://www.uptodate.com/contents/acute-coronary-syndrome-terminology-and-classification?search=acs%20terminology&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1