Nothing Humerus About It: An Approach to Shoulder Dislocations
CASE
A 52 year old male with a history of type 2 DM presented to the ED with right shoulder pain after a fall while stepping off a bus. The patient noted that he was unable to range the shoulder. Vitals were significant for HR of 104, otherwise unremarkable. On examination, the patient had a flattened shoulder with a “squared-off” appearance, a prominent acromion with the elbow flexed, and the arm held in slight abduction.
Figure 1: Shoulder Dislocation. “Shoulder Dislocation.” Core EM, coreem.net/core/shoulder-dislocation/.
DIAGNOSIS
Shoulder dislocation
DISCUSSION
IMAGING
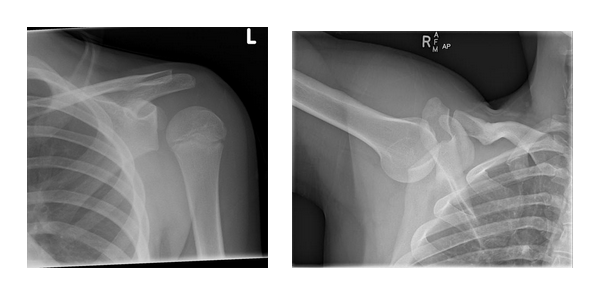
Figure 2: Initial X-rays showing anteroinferior glenohumeral dislocation
ANATOMY (AKA: Why Does This Happen So Frequently)
Shoulder dislocations comprise >50% of major joint dislocations and the frequency can largely be attributed to the joint’s underlying instability. [1] Due to how shallow the glenoid is, there is minimal articulation with the humeral head. Because of this, it relies heavily on soft tissue constraints including the labrum, glenohumeral ligaments and rotator cuff.
Figure 3. Shoulder joint anatomy
CLASSIFICATIONS
Anterior (95-97%): Further subdivided into subcoracoid and subglenoid. Often present abducted and slightly internally rotated [2]
Posterior (2-4%): Often difficult to diagnose. 34% associated with seizures [2]
Inferior (<1%): Present in fixed abduction (luxatio erecta humeri) [2]
Figure 4: First image indicating the “Lightbulb Sign” of a posterior dislocation, due to fixed internal rotation of the humeral head. Second image displaying the fixed abduction position, often present with inferior dislocations. Jones, Jeremy. “Shoulder Dislocation: Radiology Reference Article.” Radiopaedia Blog RSS, radiopaedia.org/articles/shoulder-dislocation.
ACUTE MANAGEMENT
AP, Scapula Y and axillary x-rays should all be obtained prior to reduction attempt in order to aid with planning of maneuver and to evaluate for underlying fracture. It is important to attempt reduction as early as possible as a longer time in dislocation can increase the risk of neurovascular damage and muscle spasms. Intra-articular block (often with lidocaine) should be attempted as an anesthesia technique, but procedural sedation may be required.
ASSOCIATED INJURIES
Bankart Lesion: Impaction fracture of the anterior inferior glenoid rim [3]
Hill-Sachs Lesion: Impaction fracture of the posterolateral humeral head [3]
Axillary Nerve Injury: Most commonly injured nerve in any shoulder dislocation due to its path around the surgical neck of the humerus
Rotator Cuff Tear: Should be suspected in patients with persistent pain and dysfunction after adequate reduction
Figure 5: Left AP x-ray showing both Bankart and Hill-Sachs lesions. Jones, Jeremy. “Shoulder Dislocation: Radiology Reference Article.” Radiopaedia Blog RSS, radiopaedia.org/articles/shoulder-dislocation.
COMMON ANTERIOR DISLOCATION REDUCTION TECHNIQUES
1. Cunningham:
Technique: With the patient sitting down with “chest out and shoulders back”, slowly adduct the patient’s arm and flex their elbow. You should sit/kneel directly in front of the patient so they can rest their hand on your shoulder. As you provide gentle downward traction (without abrupt pulling motions), gently massage the trapezius, deltoid and biceps sequentially with your other hand. [4] Note: this technique is gentle enough that it can be attempted without using any medication to assist in reduction, or with a dose of IV/IM analgesic +/- lidocaine joint injection.
Cons: Often does not provide a notably abrupt reduction, so must be reassessed frequently.
2. Traction / Countertraction:
Technique: With the patient supine, a sheet is wrapped under the patient’s axilla and around the chest. Pulling away from the affected side provides counter traction while a separate provider pulls the dislocated limb inferiorly and laterally at a ~45º angle. Some external rotation may be required to get past the glenoid rim [2].
Cons: Conscious sedation is typically required. Requires multiple providers.
3. Kocher:
Technique: Patient can be supine or seated. While holding the wrist and elbow on the affected side, flex the patient’s elbow to 90º with the arm adducted. Slowly externally rotate the patient’s arm until resistance (often at ~80º). At this point, provide forward flexion of the shoulder until the humeral head reduces. If resistance in the sagittal plane occurs prior to reduction, internal rotation at that time can be attempted [2].
Cons: Some studies have shown higher risks of nerve damage and humeral fracture.
4. Milch:
Technique: Patient can be supine or seated. Place your hand on the superior aspect of the affected shoulder and brace thumb over the humeral head to stabilize. With your other hand, slowly abduct the patient’s arm to an overhead position. This maneuver acts to diminish cross stresses of the muscles around the shoulder. At this point, use your thumb to slide the humeral head over the glenoid rim into anatomic position [5].
Cons: Moderately painful compared to other techniques [6]
5. Stimson
Technique: Patient should be placed in prone position with arm hanging off the stretcher. Traction should be performed by connecting 5 - 10 pounds of weight to the patient’s wrist. Over the course of the next 15-30 minutes, the patient’s shoulder should self-reduce once the deltoid and rotator cuff muscles begin to fatigue. [2]
Cons: Conscious sedation is contraindicated due to prone positioning. Additionally, some studies have shown success rates of as low as 28% without scapular manipulation. [6]
6. Scapular Manipulation
Technique: Stabilize the superior aspect of the scapula with your thumb. Using your other thumb, apply medial force to the inferior aspect of the scapula [2]. While often performed in the prone position, scapular manipulation can be combined with the Cunningham technique to good effect.
Cons: Often does not provide a notably abrupt reduction, so must be reassessed frequently.
7. FARES (Fast, Reliable, and Safe)
Technique: With the patient in a supine position, apply axial traction with the elbow extended. Perform short-range vertical oscillating movements while slowly abducting arm. External rotation can be added at 90° of abduction. Reduction often occurs at 120°. [2]
Cons: Requires higher level of technique than other maneuvers
ONE STEP FURTHER
- While some dislocations may require specific techniques due to the position of the injury, studies have shown that the majority of dislocations can be fixed with multiple techniques, so it is often left to provider preference. [7]
- Reduction of a dislocation with an accompanying fracture of the surgical neck is contraindicated, as displacement of the fracture can lead to avascular necrosis. [8] Relative contraindications include nerve deficit or chronic dislocations (higher rates of vascular complications).
- Multiple failed attempts at reduction may indicate underlying soft tissue or osseous interposition. These cases may require open surgery to receive adequate reduction. [9]
CASE RESOLUTION
Patient was anesthetized with an intra-articular lidocaine block and reduced with the Cunningham technique. Patient tolerated the procedure well and was placed in a sling. He was referred for follow-up with the orthopedics team as an outpatient. It was explained to the patient that he may require surgery if he has recurrent dislocations in the future.
Figure 6: Post-reduction X-rays confirming proper humeral position
AUTHOR: J. Kyle Volpe is a first year emergency medicine residents at Brown University / Rhode Island Hospital.
FACULTY REVIEWER: Alison Hayward, MD is an attending physician and Assistant Professor in the divisions of Education and Global Health in the Department of Emergency Medicine at Brown University
References
[1] Cunningham, N. Techniques for reduction of anteroinferior shoulder dislocation. Emergency Medicine Australasia. 2005;17(5-6);463-471
[2] Youm, T., Takemoto R., Park B. Acute Management of Shoulder Dislocations. Journal of the American Academy of Orthopaedic Surgeons: 2014;22:761-771
[3] Sheehan, S., Gaviola G., Gordon R., Sacks A., Lewis S., Smith S. American Journal of Roentgenology. 2013 201:2, 378-393
[4] Walsh, R., Harper H., McGrane O. Too good to be true? Our experience with the Cunningham method of dislocated shoulder reduction. The American Journal of Emergency Medicine: 2012;30(2);376-377
[5] Wheeless, C. Milch Technique of Shoulder Reduction [Internet]. Wheeless’ Textbook of Orthopaedics, Presented by Duke Orthopaedics. https://www.wheelessonline.com/joints/milch-technique-of-shoulder-reduction/
[6] Ibiebele, A., Ketterer, A. A Recipe for Reduction: Five alternative approaches for reducing an anterior shoulder dislocation [Internet]. NUEM Blog. https://www.nuemblog.com/blog?tag=traction-counter+traction
[7] Dannenbaum J, Krueger CA, Johnson A. A review of reduction techniques for anterior glenohumeral joint dislocations. J Spec Oper Med. 2012 Summer;12(2):83-92.
[8] Long, B. Anterior Shoulder Dislocation [Internet]. EM@3AM. http://www.emdocs.net/em3am-anterior-shoulder-dislocation/
[9] Gudena, R., Iyengar, K.P., Nadkarni, J.B., Loh, W., Irreducible shoulder dislocation – A word of caution. Orthopaedics & Traumatology: Surgery & Research: 2011;97(4);451-453