Ultrasound: Ovarian Torsion
CASE
A 24-year-old female with a past medical history of polycystic ovarian syndrome and urinary tract infections, who presented to the emergency department (ED) via urgent care with acute on chronic worsening abdominal pain and a cystic structure in the pelvis on computed tomography (CT) scan.
She described three weeks of intermittent diffuse, non-radiating, 6/10 abdominal pain without identifiable triggers but associated with anorexia, dyspareunia, dull perineal pain and mild nausea. She has not vomited, had fevers, chills, night sweats, melena or hematochezia. She hasn’t eaten any unusual foods. She continues to have bowel movements and pass gas. Gynecologic history is significant for implantation of an intrauterine device with her last menses 6 months prior, G0P0, sexually active, with no history of sexually transmitted infections. She has no previous abdominal surgeries, and her numerous workups for abdominal pain have previously ruled out celiac disease, ulcerative colitis, and Crohn’s.
Her symptoms led her to go to a urgent care site where initial testing including urinalysis was normal. A CT scan of the abdomen was performed which revealed moderate stool burden, no other GI tract pathology, and a 9.1 x 7.9 x 4.3 cm cystic structure in the posterior pelvis. At this time, the urgent care providers sent her to the ED.
During physical exam she appeared uncomfortable on the exam table, with normal heart and lung sounds. Abdominal exam revealed tenderness to light palpation throughout with guarding during deep palpation of the RLQ. On bimanual exam, she was tender to palpation of the right adnexa, no masses palpated.
In the ED, point-of-care ultrasound (POCUS) was performed.
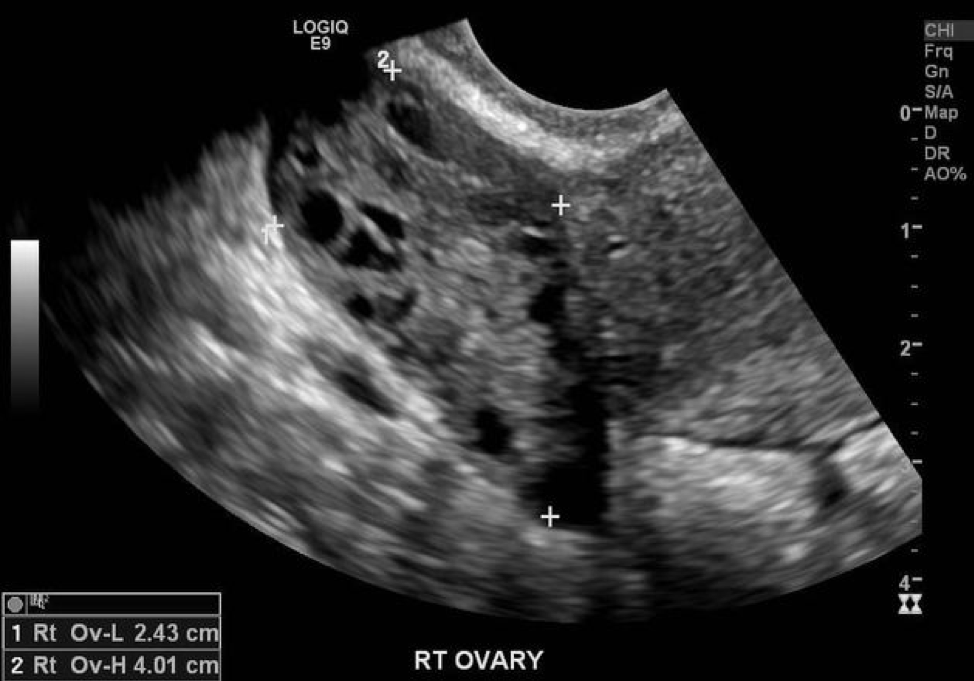
Image 1: Sample pelvic ultrasound finding. *The image above shows an enlarged ovary in setting of torsion representative of this patient case. Exact images not available as this patient was seen at outside hospital. Source: https://radiopaedia.org/cases/ovarian-torsion-detorsion.
Ultrasound revealed 9.5 x 9.1 x 4.4 cm right ovary with innumerable peripheral follicles, no sign of mass or cyst, with intact arterial and venous flow within the right ovary and twisted appearance of pedicle. Left ovary <4cm with numerous peripheral follicles. Small amount of free fluid in the cul-de-sac.
DIAGNOSIS
Intermittent ovarian torsion
DISCUSSION
Ovarian torsion is twisting of the ovary on the infundibulopelvic and utero-ovarian ligaments leading to impaired arterial inflow and lymphatic and venous drainage. This causes ovarian edema, necrosis, loss of function, and in extreme cases peritonitis. It is the fifth most common gynecologic emergency. Torsion most commonly occurs in reproductive age people with ovaries, but it can occur at any age. Risk factors for ovarian torsion include ovarian masses greater than 4 cm, cysts, long tendons, pregnancy, ovarian hyper-stimulation syndrome, and previous torsion.[1]
Signs and symptoms
Patients typically present with acute onset lower quadrant pain, adnexal mass most often on the right side, accompanied by nausea and vomiting.[1] However, clinical presentation can vary greatly. Atypical presentations include chronic, waxing and waning symptoms as in the case in intermittent torsion, or fever and abdominal pain which is more concerning for progression to necrosis.
How to approach point-of-care imaging
Transabdominal (TAUS) and transvaginal ultrasound (TVUS) are the preferred imaging modalities for ovarian torsion.[2] POCUS can reduce ED patient stay and time to consultation in non-pregnant patients with gynecologic complaints.[3] When possible, the endocavitary probe has better resolution and can allow for easier identification of pelvic structures.
For TVUS, first ensure that the indicator is toward the ceiling, and gently insert the probe. Identify the endometrial stripe. Scan the uterus by rotating the transducer and adjust the probe to sit against the adnexa. Look for ovoid shape of ovaries with hypoechoic follicles. Remember your landmarks - the iliac vessels and the cornual region of the uterus.
The most common ultrasound finding of torsion is unilateral ovarian enlargement (> 4 cm). Additional findings are ovarian edema due to vascular congestion (hypoechoic), peripherally displaced follicles, and free fluid in the pelvis.[2] Abnormal or reduced ovarian Doppler flow was seen in only ~50% of patients in one study, therefore presence of vascular flow does not rule out torsion.[4] The “whirlpool sign,” in which coiled or circular vessels are visualized without Doppler flow within a tubular or beaked mass (the pedicle) on gray scale, supports diagnosis of torsion.[5]
If you are unable to obtain adequate images and your index of suspicion for torsion remains high, proceed with work-up as absence of POCUS findings is not sufficient to rule out torsion.
Concise guides to transvaginal POCUS can be found here (specific to ovarian torsion), here and here (generic).
Image 2: Normal ovary on transvaginal ultrasound. Image source: https://wikem.org/wiki/Pelvic_ultrasound_(transvaginal)
Image 3: Sample transvaginal ultrasound findings in ovarian torsion including enlarged ovary with peripherally displaced follicles and free fluid. Image Source: https://www.acep.org/how-we-serve/sections/emergency-ultrasound/news/september-2020/ovarian-torsion/
Image 4: Whirlpool sign as seen in transabdominal imaging. Image source: Vijayaraghavan et al 2004.[5]
Diagnosis, treatment, and prognosis
Ovarian torsion is diagnosed surgically with direct visualization. Therefore, the role of the emergency physician is to identify patients whose presentation is suspicious for torsion and appropriate for gynecology consult and intervention. After ruling out other causes of pelvic pain; a combination of signs, symptoms, and ultrasound findings are sufficient for a clinical diagnosis of ovarian torsion. Pelvic exam without adnexal mass should not lower suspicion for torsion due to low inter-examiner reliability in identifying mass in setting of torsion. Urgent surgical evaluation for diagnosis and de-torsion is performed laparoscopically to assess for viability of the ovary and determine presence of mass or cyst in need of intervention, need for resection of necrotic tissue, oophorectomy, or oopheropexy.[6]
CASE RESOLUTION
Our patient was taken to the operating room and found to have 1080-degree rotation of the right ovary and was noted to have long ovarian ligaments. Detorsion and bilateral oopheropexy was performed. Patient went on to have two additional oopheropexy procedures with ligament shortening and resection of a portion of the right ovary due to recurrent torsion despite initial oopheropexy. Her history of five years of intermittent abdominal pain was believed to be attributable to intermittent torsion.
TAKE-AWAYS
Ovarian torsion should be considered in people of reproductive age with ovaries presenting with abdominal or pelvic pain.
On ultrasound, torsion most commonly appears as unilaterally enlarged, edematous ovary, but can also appear more specifically with the “whirlpool sign” or “follicular ring sign.”
Presence of Doppler flow in ovary does not rule out torsion.
AUTHOR: Sarah Kler, 4th year medical student at Albert Medical School of Brown University
FACULTY REVIEWERr: Kristin Dwyer, MD MPH, Assistant Professor Brown University, Director of Emergency Ultrasound Division, Director Emergency Ultrasound Fellowship.
REFERENCES
Houry D, Abbott JT. (2001), Ovarian torsion: a fifteen-year review. Ann Emerg Med. 38:156-159. https://doi.org/10.1067/mem.2001.114303
Priyadarshani et al. ACR Appropriateness Criteria® Acute Pelvic Pain in the Reproductive Age Group. Available at https://acsearch.acr.org/docs/69503/Narrative/. American College of Radiology. Accessed Feb 24 2020.
Wilson, S. P., Connolly, K., Lahham, S., Subeh, M., Fischetti, C., Chiem, A., Aspen, A., Anderson, C., & Fox, J. C. (2016). Point-of-care ultrasound versus radiology department pelvic ultrasound on emergency department length of stay. World journal of emergency medicine, 7(3), 178–182. https://doi.org/10.5847/wjem.j.1920-8642.2016.03.003
Moro, F., Bolomini, G., Sibal, M., Vijayaraghavan, S.B., Venkatesh, P., Nardelli, F., Pasciuto, T., Mascilini, F., Pozzati, F., Leone, F.P.G., Josefsson, H., Epstein, E., Guerriero, S., Scambia, G., Valentin, L. and Testa, A.C. (2020), Imaging in gynecological disease (20): clinical and ultrasound characteristics of adnexal torsion. Ultrasound Obstet Gynecol, 56: 934-943. https://doi-org.revproxy.brown.edu/10.1002/uog.21981
Vijayaraghavan, S.B. (2004), Sonographic Whirlpool Sign in Ovarian Torsion. Journal of Ultrasound in Medicine, 23: 1643-1649. https://doi.org/10.7863/jum.2004.23.12.1643
Oelsner G, Cohen SB, Soriano D, Admon D, Mashiach S, Carp H. (2003), Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod. 18(12):2599-602. https://doi: 10.1093/humrep/deg498.
To learn more:
https://emlyceum.com/2012/06/21/ovarian-torsion-answers/


![Image 4: Whirlpool sign as seen in transabdominal imaging. Image source: Vijayaraghavan et al 2004.[5] ](https://images.squarespace-cdn.com/content/v1/56e8a86a746fb97ea9d14740/1614973252153-2Z69HLE3939DZS03O6RQ/whirlpool.png)