Renal Ultrasound: Hydronephrosis and Stones
Flank pain is a very common presenting complaint for visits in the emergency department (ED), accounting for over two million annual ED visits. [1] While the differential is broad, when one sees this listed as the chief complaint, you may as well bring the ultrasound machine in with you when you go to assess the patient. Renal ultrasound can be important in determining diagnosis, management, and next steps in the evaluation of a patient with flank or abdominal pain, hematuria, concern for stone and more.
Discussion:
Scan Technique:
A curvilinear or phased array transducer are the best options for a renal ultrasound given their capability for high penetration. [2] On the patient’s right side, the probe should be placed in the midaxillary line between the 9th- 11th rib. Meanwhile, on the patient’s left, the probe will be in the posterior axillary line between the 8th to 10th rib space. Keep in mind that the probe will need to be rotated slightly obliquely, to minimize rib shadow. You should scan through the entire kidney slowly on both sides in both the coronal and the transverse planes. Apply color doppler to differentiate between the collecting system, which will not exhibit color flow, and the renal vasculature.
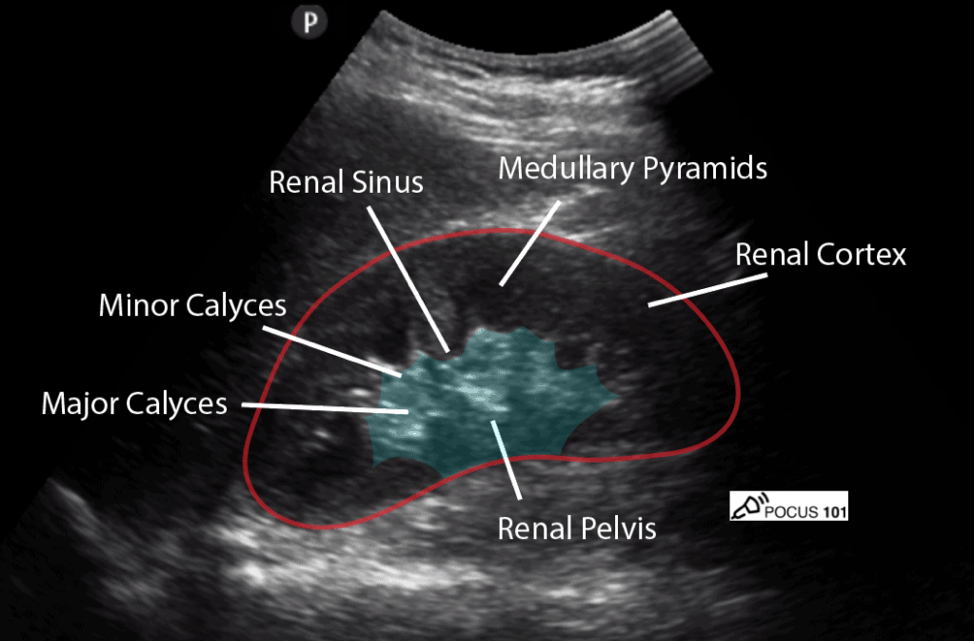
Normal Kidney on US:
A normal kidney will be surrounded by a capsule, which appears as a bright white, hyperechoic line on ultrasound. Each kidney’s cortex will usually be 1cm thick and on ultrasound will appear like a liver in terms of echogenicity. The kidney’s medullary pyramids will appear as dark, hypoechoic wedges on ultrasound. Important to note that in a normal kidney these pyramids are non-communicating, existing as discrete hypoechoic wedges separated from one another. Lastly, renal calyces merge to form a renal pelvis which normally appear as collapsed and hyperechoic.
FIGURE 1: NORMAL APPEARANCE OF KIDNEY ON ULTRASOUND [3]
Hydronephrosis is swelling in the kidney due to backup of urine; often from an internal blockage of the ureter (such as in renal colic) or extrinsic pressure and blockage on the ureter (such as from a malignancy, or abdominal aortic aneurysm).
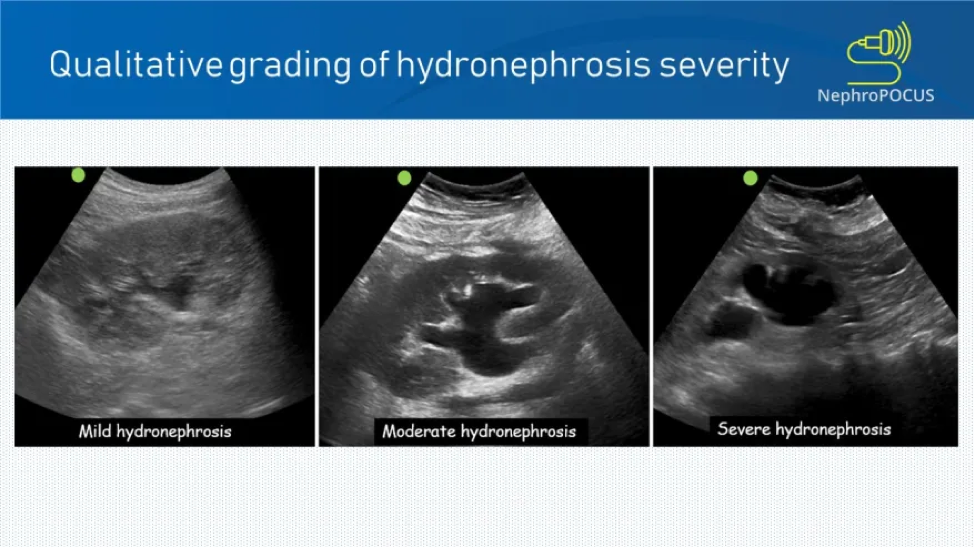
There are various grades of hydronephrosis:
Mild: In mild hydronephrosis, the renal pelvis will appear fluid filled, though the calyces are likely still collapsed. In pregnancy, mild hydronephrosis can be a normal finding. This is also true if the patient is in a state of urinary retention or has an extremely full bladder.
Moderate: The calyces in this state will now appear to be open, this is often referred to as a “Bear’s Paw” due to the dilated collecting system.
Severe: In this state, the calyces will appear largely filled with fluid and will appear to coalesce due to swelling. The calyces will appear rounder and more blunted. The medulla and the pyramids will no longer be visualized.
FIGURE 2: GRADING OF HYDRONEPHROSIS ON ULTRASOUND [4]
Kidney stones appear hyperechoic (white) on ultrasound, often coupled with posterior shadowing. The posterior shadowing helps to distinguish stones from normal kidney anatomy which may also appear bright white. Twinkling artifact, a useful finding when color Doppler is used, is highly suggestive of renal stones as can be appreciated in Figure 3. This can be useful when there is a smaller stone which may not have been visualized. It is important to note that renal ultrasound does not image the ureters. Ureteral stones may also be a source obstruction despite not being displayed on imaging of the kidney. However, ultrasound is 90% sensitive for detecting the hydronephrosis which can be caused by ureteral stones. [5]
FIGURE 3: TWINKLE ARTIFACT ON ULTRASOUND[6]
Although computer tomography (CT) may also be used as an imaging tool in detecting hydronephrosis and nephrolithiasis, ultrasound has been found to be effective. [7] Initiating kidney imaging with ultrasound was “associated with lower cumulative radiation exposure than initial CT”. [7] In addition, there were no significant differences in “high-risk diagnoses with complications, serious adverse events, pain scores, return emergency department visits, or hospitalizations” between initiating with ultrasound versus CT. [7] Common pitfalls on ultrasound include misidentifying the renal vessels or medullary pyramids for hydronephrosis.
Although a patient with renal colic may exhibit a range of hydronephrosis on a bedside ultrasound, it is still very helpful information to guide your next steps. A patient who you are fairly certain has a kidney stone, and exhibits none or mild hydronephrosis, maybe able to go home once pain controlled and tolerating PO with a normal urinalysis and creatinine. Patients without infection and no significant obstruction are very likely to pass their stone on their own and are less likely to need advanced imaging unless you are concerned for alternative dangerous abdominal pathology. In contrast, a patient with moderate to severe hydronephrosis, or with evidence of a urinary tract infection may require a urologic consultation and potentially advanced imaging for interventional planning (eg how large and how proximal is the stone). Be sure to also consider evaluation of the aorta with your ultrasound, as patients with flank pain and hydro may have a large AAA, which is a can’t-miss diagnosis.
Summary/Take-Away
Hydronephrosis can be caused by an internal blockage or external compression.
It is important to keep AAA on your differential. When you are imaging the kidney, make sure to image the aorta as well to rule in or rule out a AAA.
Kidney stones will appear hyperechoic on imaging, often accompanied by posterior shadowing, however, you are primarily looking for evidence of obstruction in the ureter (eg hydronephrosis), not necessarily the stone itself.
When a patient presents with flank pain, and is diagnosed with a stone without significant obstruction, make sure their pain is controlled and that they tolerate PO and do not have a urinary tract infection before discharge.
Keywords:
Flank pain, hydronephrosis, kidney stones, abdominal pain
AUTHOR: Naomie Shembo
FACULTY REVIEWER: Kristin Dwyer, MD
References
Moore, C. L., Carpenter, C. R., Heilbrun, M. E., Klauer, K., Krambeck, A., Moreno, C., Remer, E. M., Scales, C., Shaw, M. M., & Sternberg, K. M. (2019). Imaging in suspected renal colic: Systematic review of the literature and Multispecialty Consensus. Annals of Emergency Medicine, 74(3), 391–399. https://doi.org/10.1016/j.annemergmed.2019.04.021
AEUS. (2021, October 8). Renal ultrasound. Vimeo. Retrieved December 17, 2021, from https://vimeo.com/69556457
Dinh, V. (n.d.). Renal Ultrasound Made Easy: Step-by-step guide. POCUS 101. Retrieved December 17, 2021, from https://www.pocus101.com/renal-ultrasound-made-easy-step-by-step-guide/
Koratala, A. (2020, August 12). Hydronephrosis. NephroPOCUS. Retrieved December 17, 2021, from https://nephropocus.com/2019/05/31/hydronephrosis/
Gaspari, R. J., & Horst, K. (2005). Emergency ultrasound and urinalysis in the evaluation of Flank pain. Academic Emergency Medicine, 12(12), 1180–1184. https://doi.org/10.1197/j.aem.2005.06.023
Carbonatto, G. (2021, August 10). Renal colic - the twinkle artifact. Critical Care Sonography. Retrieved December 17, 2021, from https://www.criticalcare-sonography.com/2017/04/08/renal-colic-the-twinkle-artifact/
Smith-Bindman, R., Aubin, C., Bailitz, J., Bengiamin, R. N., Camargo, C. A., Corbo, J., Dean, A. J., Goldstein, R. B., Griffey, R. T., Jay, G. D., Kang, T. L., Kriesel, D. R., Ma, O. J., Mallin, M., Manson, W., Melnikow, J., Miglioretti, D. L., Miller, S. K., Mills, L. D., … Cummings, S. R. (2014). Ultrasonography versus computed tomography for suspected nephrolithiasis. New England Journal of Medicine, 371(12), 1100–1110. https://doi.org/10.1056/nejmoa1404446