Soft Tissue Infection: Diagnosis by Ultrasound
CASE
A 31 y.o. male presents to the Emergency Department with a chief complaint of swelling of his right leg. He has no past medical history, and his social history is significant for polysubstance use disorder and housing insecurity. He primarily injects opioids and cocaine and has had periods of time where he received medication assisted treatment with buprenorphine. On exam, there is an area of erythema and swelling on the lower right extremity that does not overly the joints. The area is warm and tender to palpation. There is no obvious wound or purulent drainage. The remainder of a 12 point Review of Systems is negative.
Vitals:
T: 99.0
HR: 85
BP: 135/90
RR: 20
Sat: 97% on room air
A bedside ultrasound of the area was performed which showed fluid stranding in the subcutaneous soft tissue as well as a discrete, walled, fluid collection with hyperdense intracavitary material.
Image 1. Ultrasound depicting soft tissue stranding with abscess.
DIAGNOSIS
A diagnosis of cellulitis with abscess was made based on history, exam, and ultrasound findings. The patient was treated with incision and drainage of the observed fluid collection, prescribed a 7-day course of doxycycline 100mg twice daily, and provided resources by a social worker and community health worker. The patient declined consultation with addiction medicine and was discharged with alcohol wipes, sterile water, hydrogen peroxide, sterile gauze, sterile needles, sterile syringes, directions to a supervised consumption facility.
DISCUSSION
Soft tissue infections represent a spectrum of disease. Some infections can be managed with observation and/or antibiotics in cases of simple cellulitis, but others may require management with incision and drainage or placement of a drain. Rapidly making decisions about soft tissue infection management is a frequent challenge for emergency medicine (EM) physicians made easier and more efficient with use of bedside ultrasound.
Specifically, ultrasound allows clinicians to answer important questions at the bedside with minimal delay when presented with a soft tissue infection.
Is there a fluid pocket that should be drained?
Is this a necrotizing infection by gas forming bacteria?
Is there a retained foreign body?
Does this infection extend to deep space?
Do I need cross sectional imaging and/or surgical consultation?
Image 2. “Cobblestone” pattern on ultrasound.
Cellulitis is well visualized on ultrasound as a “Cobblestone” pattern (Image 2). This cobblestone pattern is produced by fluid tracking between the adipose and fasciae as a result of increased vascular permeability and inflammation driven by infection. [1,2]
Image 3. Abscess visualized on ultrasound.
Abscess is visualized as a discrete collection of subcutaneous fluid. Fibrinous loculations or proteinaceous inflammatory debris may be visualized as in the image above (Image 3). There may be associated cellulitis, however some abscesses present in the absence of cellulitis. Ultrasound has been shown to have a sensitivity of 97% and specificity of 83% in diagnosis of abscess in soft tissue infection. [3] In addition, the use of ultrasound has been shown to lead to changes in management in potentially as many as 56% of cases of soft tissue infection considered. [4,5] Ultrasound has been shown to be more accurate than clinical exam alone in diagnosis of abscess. [6] Lastly, ultrasound has been shown to be more sensitive for abscess than CT, though CT is shown to be more specific in diagnosis of abscess. [7]
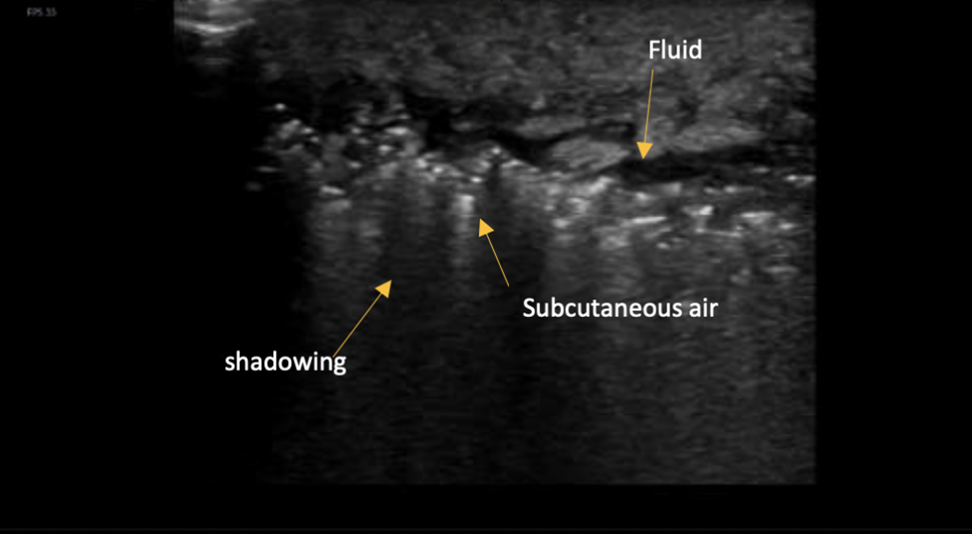
Image 4. Scattered soft tissue hyper-echoic areas representing subcutanous air.
Necrotizing fasciitis is a life-threatening soft tissue infection by gas forming bacteria. The infection is rapidly progressive and necessitates rapid diagnosis to minimize morbidity and mortality. Subcutaneous air is a hallmark of the diagnosis and is appreciated on ultrasound by the presence of scattered soft tissue hyperechoic areas as shown above (Image 4). In the literature, ultrasonography has been shown to have a sensitivity of 88% and a specificity of 93% for necrotizing fasciitis. [8]
For more in-depth review of Ultrasound in diagnosis of necrotizing fasciitis, please see:
http://brownemblog.com/blog-1/2020/7/23/necrotizing-soft-tissue-infection-diagnosis-with-ultrasound
Common infections and Etiologies:
Staph Aureus (MSSA and MRSA) and Streptococcus pneumoniae are the most common organisms.
Common risk factors for the development of soft tissue infection include:
Trauma with violation of the dermis
Intravenous drug use
Barriers to hygiene including housing insecurity and social/medical neglect
Diabetes
Kidney disease
Liver disease
HIV/AIDS
Transplant patients
Patient on active chemotherapy
Any patient taking immunosuppressive therapy (Lupus, MS etc.)
Patients with dermatological disease (Acne, Hydrenitis supritiva, pilonidal cyst, bartholin cyst, ingrown hairs, etc.)
Probe and Machine Considerations
Image 5. LInear (high frequency) ultrasound probe
The linear probe is ideal for assessing soft tissue. Higher frequencies allow for excellent resolution at a shallow depth. While use of this probe offers better image resolution, depth of penetration is limited. If unable to visualize the extent of disease with the linear probe, consider using a different probe or cross sectional imaging with CT.
TAKE-AWAYS
Ultrasound is a valuable tool for assessing the spectrum of soft tissue infections. Use of the high-frequency linear probe allows assessment with high specificity and sensitivity for differentiating cellulitis, abscess, and necrotizing fasciitis. Use of ultrasound commonly results in changes in clinically significant changes in management of soft tissue infection.
AUTHOR: Keaton Cameron-Burr, MD is a second year emergency medicine resident at Brown University/Rhode Island Hospital.
FACULTY REVIEWER: Kristin Dwyer, MD is Assistant Professor of Emergency Medicine and Emergency Ultrasound Fellowship Director at Brown Emergency Medicine.
REFERENCES
Tayal, V.S., Hasan, N., Norton, H.J. and Tomaszewski, C.A. (2006), The Effect of Soft-tissue Ultrasound on the Management of Cellulitis in the Emergency Department. Academic Emergency Medicine, 13: 384-388.
Radswiki, T., Knipe, H. Cellulitis. Reference article, Radiopaedia.org. (accessed on 25 May 2022)
Subramaniam S, Bober J, Chao J, Zehtabchi S. Point-of-care Ultrasound for Diagnosis of Abscess in Skin and Soft Tissue Infections. Acad Emerg Med. 2016 Nov;23(11):1298-1306.
Alsaawi A, Alrajhi K, Alshehri A, Ababtain A, Alsolamy S. Ultrasonography for the diagnosis of patients with clinically suspected skin and soft tissue infections: a systematic review of the literature. Eur J Emerg Med. 2017 Jun;24(3):162-169.
Tayal, V.S., Hasan, N., Norton, H.J. and Tomaszewski, C.A. (2006), The Effect of Soft-tissue Ultrasound on the Management of Cellulitis in the Emergency Department. Academic Emergency Medicine, 13: 384-388.
Squire, B.T., Fox, J.C. and Anderson, C. (2005), ABSCESS: Applied Bedside Sonography for Convenient Evaluation of Superficial Soft Tissue Infections. Academic Emergency Medicine, 12: 601-606.
Gaspari, R., Dayno, M., Briones, J. et al. Comparison of computerized tomography and ultrasound for diagnosing soft tissue abscesses. Crit Ultrasound J 4, 5 (2012).
Yen, Z.-S., Wang, H.-P., Ma, H.-M., Chen, S.-C. and Chen, W.-J. (2002), Ultrasonographic Screening of Clinically-suspected Necrotizing Fasciitis. Academic Emergency Medicine, 9: 1448-1451.