ED Approach To Dizziness
CASE
A 55 year-old-male presents to the emergency department complaining of dizziness. He has a past medical history of alcoholic cirrhosis (now sober for the past 4 years) and hypertension and is an active 1 pack/day smoker. His symptoms started the night after his second Covid vaccine two weeks ago, when he began to feel unsteady while walking. He also reports morning nausea and headaches which are relieved when he drinks coffee and takes aspirin. He believes that his symptoms were a result of his vaccine or his recent dental procedures, but his dentist said this was unlikely. His family has been concerned about his ongoing symptoms, and his wife convinced him to come in today after he tripped while carrying groceries.
DISCUSSION: Approach to “Dizziness”
The first step in approaching a patient who presents with “dizziness” is to fit this non-specific complaint into a more precise category. The history is often sufficient to identify the etiology but physical exam can also contribute to the diagnosis if there are positional changes in symptoms, orthostatic blood pressure changes, nystagmus or gait abnormalities. Key characteristics of different types of dizziness include:
Vertigo: Arising from problems with the vestibular system, patients will describe a feeling of motion (either of themselves or their environment) while at rest. They classically describe a “spinning” sensation, but this is not required for a diagnosis of vertigo. It is usually provoked by certain changes in position or middle ear pressure and is always made worse by movement of the head. Nystagmus is a common associated symptom.
Disequilibrium: This sense of imbalance, primarily while walking, has a number of causes including peripheral neuropathies, cerebellar and vestibular disorders, and musculoskeletal disorders. Associated symptoms of limb incoordination, nystagmus, or postural hypotension may be helpful in distinguishing between these causes.
Pre-syncope: Patients can usually recognize this as a few seconds to minutes of feeling like they are about to faint, but less severe episodes can include lightheadedness, feelings of warmth, diaphoresis, nausea, and blurred vision.
Other/nonspecific dizziness: Some patients cannot describe their dizziness further and do not fall easily into one of the above categories. Psychiatric disorders, hyperventilation, and mild versions of vertigo or presyncope can be the primary cause of nonspecific dizziness.
CASE CONTINUED
Upon further questioning, our patient denies any visual changes, speech difficulties, numbness, weakness, or paresthesias. He explains that he has felt unsteady on his feet and clumsier than normal, but has not experienced vertigo. On exam, he is hypertensive (140/100), but vital signs are otherwise normal. He is well-appearing and in no acute distress. Alert and oriented to person, place and time.
On neurologic exam, he has intact facial sensation, smile and brow raise bilaterally. His extraocular movements are intact without nystagmus. There is no pronator drift. Strength is 5/5 in the arms and legs bilaterally with symmetric shoulder shrug. He has a negative Babinski sign and intact proprioception of the great toes. There is mild dysmetria with finger-to-nose testing bilaterally, with the right worse than the left.
Based on his description of his symptoms and his exam finding of dysmetria, his dizziness can be better characterized as disequilibrium with a possible cerebellar etiology. At this time, an emergent brain CT was ordered to rule out posterior stroke as well as other acute intracranial processes.
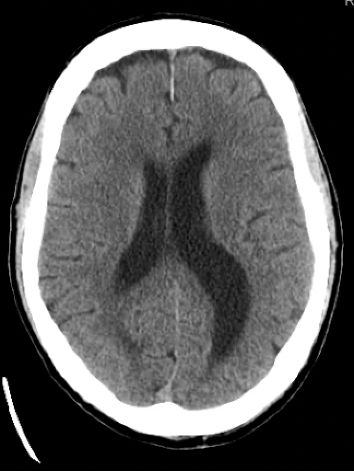
The CT brain showed a 4.5 cm left cerebellar mass, associated with moderate cerebellar edema, sulcal effacement and left to right cerebellar midline shift. An additional 1.2 cm mass was identified in the pons.
Figure 1. CT findings demonstrating cerebellar mass with edema and midline shift
The neuroimaging finding of midline shift represents significantly increased intracranial pressure, which must be treated emergently to prevent life-threatening herniation. In this case, where mass effect and peritumoral edema are the cause, systemic glucocorticoids should be the first-line treatment to stabilize patients until definitive management of the tumor is possible. Dexamethasone is the standard agent because it is highly potent and has low mineralocorticoid activity and thus will not cause much fluid retention.
This patient also needs to be transferred to a hospital where neurology, critical care and neurosurgery resources are available. While the urgency of neurosurgery evaluation varies among patients with new brain tumor diagnoses, those with signs of elevated ICP or impending herniation require emergent attention.
The patient was transferred to a hospital with neurosurgery capacity, where he underwent neurosurgical evaluation and was admitted to the neuro ICU. During his subsequent hospital stay, a CT of his chest, abdomen and pelvis demonstrated two masses in the left upper lobe of the lung, which likely represent the primary malignancy.
Figure 2. CT findings of lung mass
A bronchoscopy with biopsy and suboccipital craniotomy were performed and confirmed the diagnosis of metastatic carcinoma.
Author: Katherine Barry is a fourth-year medical student at the Warren Alpert Medical School of Brown University.
Faculty Reviewer: Kristina McAteer, MD is an attending physician at Rhode Island Hospital and Newport Hospital.
REFERENCES
“Approach to the Patient with Dizziness.” UpToDate, www.uptodate.com/contents/approach-to-the-patient-with-dizziness?search=dizziness&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1.
“Management of Vasogenic Edema in Patients with Primary and Metastatic Brain Tumors.” UpToDate, www.uptodate.com/contents/management-of-vasogenic-edema-in-patients-with-primary-and-metastatic-brain-tumors?search=brain+mass+edema+shift&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H2211992301.
Overview of the Clinical Features and Diagnosis of Brain Tumors in Adults.” UpToDate, www.uptodate.com/contents/overview-of-the-clinical-features-and-diagnosis-of-brain-tumors-in-adults?search=new+brain+mass&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H1415435983.