Postmortem Applications of Medical Imaging
A 50-year-old woman with a history of cancer with pulmonary metastases presented for outpatient lung biopsy. The biopsy was performed, and after the first specimen was obtained, the patient had massive hemoptysis requiring suctioning. Her blood oxygen level began to decline and a rapid response was called followed by a code blue. After being intubated, the patient went into pulseless electrical activity and received multiple rounds of epinephrine and sodium bicarbonate, and one shock for ventricular fibrillation. She ultimately went back into pulseless electrical activity arrest and was soon pronounced dead. An autopsy was requested by family.
The autopsy started by reviewing the patients CT images captured during the needle biopsy to locate the nodule within the lung and the procedure site. A few CT images captured the nodule, needle insertion, and areas of possible hemorrhage. However, little could be ascertained regarding the precise source or extent of the bleed. No images were captured after the hemorrhage began as the team was providing care to the patient.
Per autopsy protocol, a full external exam was conducted, but the location of the needle entry site was difficult to identify due to livor mortis in dependent areas of the decedent’s back. A full thoracic autopsy had been requested and would entail a deliberate opening of the chest cavity, careful measuring of the effusion and hemorrhage volumes and locations, and removal of the heart and lungs with dissection and tissue sampling of standard and pathological anatomy.
External examination of decedent searching for needle aspiration site.
This is a very thorough and standardized procedure, but I found myself wondering if there may be additional information about the hemorrhage that could be gained prior to disrupting the tissue or some clues that may be lost as we dissected the tissue. The needle site was difficult to appreciate externally, and the architecture and needle path would be rotated and separated from surrounding layers during the removal of the lung. What caused such an unusual outcome in such a standard biopsy procedure? Was this an overly vascularized nodule? Was a nearby artery involved in the hemorrhage?
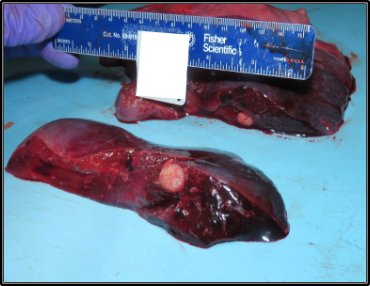
Decedent’s right lung showing hemorrhage and biopsy nodule.
Autopsy is from the Greek “autopsia” which means “the act of seeing for oneself.” The first clinically correlated postmortem exam was conducted in the second century BCE by Galen of Pergamum in Greece. The autopsy procedure itself has changed very little over time. As I thought how much technology has improved since humans first conducted autopsies, I wondered what other tools might be available to help us “to see” prior to dissecting specimens. I began to research the utility of our current medical imaging tools in postmortem examinations.
There are a few common uses of imaging in postmortem examination. For instance, pediatric and perinatal pathology commonly use x-rays in autopsies for determining age from femur length and detecting skeletal anomalies. But despite the many benefits postmortem imaging offers, many applications are not routine in practice. When families do not consent to an autopsy, many clinical questions may be left unanswered. But imaging could serve as an adjunct and alternative to full conventional autopsy, offering a less invasive means of visualizing pathology. The ability to provide some answers with imaging as a form of limited autopsy may be more acceptable to many families and could provide answers and closure.
X-ray provides excellent postmortem imaging of foreign bodies, fractures, and trauma, and can also provide dental identification and insights when decomposition has taken its toll in forensic pathology cases. The drawbacks are its limited ability to visualize soft tissue and organs, its high upfront maintenance and technician costs, and the machine’s relatively large size which would usually require a decedent to be transported from the morgue to an imaging suite. CT offers many of the same benefits and drawbacks to X-ray but also adds the capability of visualizing soft tissue, gas, and fluids. These make CT advantageous in ballistics, traumas, child abuse, identification, air embolisms, vascular imaging, and decomposition cases. Finally, postmortem MRI offers excellent soft tissue, brain, and spinal cord imaging, and also provides accurate estimation of organs. This makes MRI useful for visualizing traumatic and medical organ lesions, strangulation, child abuse, and skeletal age estimation. However, postmortem MRI has poor accuracy for heart, lung, and bladder lesions. Additionally, MRI machines have a very high purchase and operating cost, they are the largest of the imaging devices, and they require special architecture for the electromagnet use. Like X-ray and CT, MRI would also require the decedent to be transported from the hospital morgue to the imaging suite, which is time consuming and labor intensive.
Postmortem ultrasound has been studied as a minimally invasive adjunct to autopsy as recently as 2021 during the Covid-19 pandemic by Brook et al. Ultrasound offers good soft tissue, organ, and fluid imaging. It is more practical than other imaging modalities as the ultrasound can be brought to the morgue rather than transporting the decedent. It is safe to use with no radiation and is significantly less expensive. Ultrasound also offers the benefit of being used by a trained pathologist rather than requiring a technician and or radiologist to interpret the image. It therefore offers real-time imaging that can guide a complete autopsy and provide further insight at various stages during the whole-body autopsy and organ dissection. While ultrasound does have limitations, this portable, inexpensive technology has many potential uses including for fetal autopsies, localizing masses, fluids, air, and foreign bodies, organ structure, and to guide assessment and biopsy of these structures prior to disturbing the tissue with dissection.
When comparing the many imaging modalities available today in medicine, there seem to be clear advantages to being able to use imaging technologies to assist pathologists with answering complex clinical questions in the postmortem setting. Each type of imaging has its distinct advantages and disadvantages. When weighing the cost, portability, and time delay against the need to visualize internal structures in real time in the morgue, ultrasound seems like a cost-effective tool that could offer quick insights and could also help to answer questions for families who are reluctant to consent to full autopsy. The cost of ultrasound is significantly lower than other imaging modalities, with GE’s Vscan Air merely five thousand dollars compared to an MRI machine ranging between one and three million dollars. The use of ultrasound in pathology is an exciting area in need of more exploration and study. The portability and low cost of point-of-care ultrasound are attributes that have encouraged its use all throughout medicine, and its adoption for use during the last exam a patient ever undergoes should be no exception.
Author: Bob Barno is a fourth year medical student at The Warren Alpert Medical School of Brown University
Faculty Reviewer: Kristin Dwyer, MD, MPH
References
Imaging and Virtual Autopsy: looking backward and forward- Stephan A. Bollinger et. al. NCBI, NLM, NIH. Gov, 2015.
Modern Post Mortem Imaging: an update on recent developments. Silke Grabherr. NCBI, NLM, NIH. Gov, 2017.
Virtopsy: a feasibility study. Thali et al 2003
Postmortem X-ray, CT and Forensic Autopsy: A review of utility, the challenges and future implications.
Perinatal Post-Mortem Ultrasound (PMUS). Radiological-pathological Correlation. Susan C. Shemerdine. Insights Imaging 2019.
Ultrasound Guided Minimally Invasive Autopsy as a tool for rapid port mortem diagnosis in the 2018 Sao Paulo Yellow Fever epidemic. Amaro Nunes Duarte-Nelo. Public Library of Science.
Postmortem Imaging-Guided Biopsy as an Adjuvant to Minimally Invasive Autopsy With CT and Postmortem Angiography: A Feasibility Study. Stephan A Bollinger et al. American Journal of Roentgen Ray Society. 2010
Diagnostic accuracy of post-mortem CT with targeted coronary angiography versus autopsy for coroner-requested post-mortem investigations: a prospective, masked, comparison study. Rutty et al. The Lancet volume 390, Issue 10090, July 2017
Nouma, Youssef & Ben Amar, Wiem & Zribi, Malek & Bardaa, S. & Hammami, Z. & Maatoug, Sameh. (2016). Forensic examination after exhumation: Contribution and difficulties after more than thirty years of burial. Journal of Forensic and Legal Medicine. 44. 10.1016/j.jflm.2016.10.005.
Addison S, Arthurs OJ, Thayyil S. Post-mortem MRI as an alternative to non-forensic autopsy in foetuses and children: from research into clinical practice. Br J Radiol. 2014 Apr;87(1036):20130621. doi: 10.1259/bjr.20130621. PMID: 24288400; PMCID: PMC4067011.
Javier An ̃on, MD et al. Traumatic Extra-Axial Hemorrhage: Correlation of Postmortem MSCT, MRI, and Forensic-Pathological Findings. JOURNAL OF MAGNETIC RESONANCE IMAGING 28:823–836 (2008)
Fariña J, Millana C, Fdez-Aceñero MJ, Furió V, Aragoncillo P, Martín VG, et al.. Ultrasonographic autopsy (echopsy): a new autopsy technique. Virchows Arch 2002; 440: 635–9. doi: 10.1007/s00428-002-0607-z
X. Kang, S. Postmortem examination of human fetuses: comparison of two-dimensional ultrasound with invasive autopsy. Published online 7 January 2019 in Wiley Online Library. DOI: 10.1002/uog
Brook OR, Piper KG, Mercado NB, Gebre MS, Barouch DH, Busman-Sahay K, Starke CE, Estes JD, Martinot AJ, Wrijil L, Ducat S, Hecht JL. Feasibility and safety of ultrasound-guided minimally invasive autopsy in COVID-19 patients. Abdom Radiol (NY). 2021 Mar;46(3):1263-1271. doi: 10.1007/s00261-020-02753-7. Epub 2020 Sep 17. PMID: 32939636; PMCID: PMC7494380.
Silke Grabherr, Coraline Egger, Raquel Vilarino, Lorenzo Campana, Melissa Jotterand & Fabrice Dedouit (2017) Modern post-mortem imaging: an update on recent developments, Forensic Sciences Research, 2:2, 52-64, DOI: 10.1080/20961790.2017.1330738
Wagensveld IM, Hunink MGM, Wielopolski PA, van Kemenade FJ, Krestin GP, Blokker BM, et al. (2019) Hospital implementation of minimally invasive autopsy: A prospective cohort study of clinical performance and costs. PLoS ONE 14(7): e0219291. https://doi.org/10.1371/journal.pone.0219291
Kottner, S., Schulz, M.M., Berger, F. et al. Beyond the visible spectrum – applying 3D multispectral full-body imaging to the VirtoScan system. Forensic Sci Med Pathol 17, 565–576 (2021). https://doi.org/10.1007/s12024-021-00420-x
Photo Credit: GE POCUS https://www.mmemed.com/ge-ultrasounds/ge-healthcare-vscan-air-cl-probe-h45611ch/?ppc_keyword=&gclid=EAIaIQobChMI35LAs7mI-QIVDbqGCh1RhAgvEAkYAyABEgLrLvD_BwE
Melissa Rohman. JAMA: U.S. spends the most on healthcare—and imaging is a reason why. Practice Management. March 14, 2018