Abnormal Pulses and Pulse Oximetry: Diagnosis of A Critical Congenital Heart Defect in the Emergency Department
“Wile on initial history, this patient’s gradual tachypnea in the setting of a known close sick contact may have suggested an infectious etiology, his exam including diminished femoral pulses, lack of congestion, cardiac gallop, and asymmetric pulse oximeter readings between extremities was concerning for cardiogenic anomalies…”
Case
A seven-day old male presented to the Emergency Department (ED) with twelve hours of increased work of breathing. His mother reported a healthy pregnancy and spontaneous vaginal delivery. She noted they had been home for 5 days from the newborn nursery. However, overnight she found the patient had increased work of breathing and difficulty with feeds. She noted he was no longer able to finish a full feed. She tried suctioning his nose without significant improvement. The patient’s mother also noted that another caretaker of the infant had upper respiratory symptoms. On exam, the patient’s vitals were notable for respiratory rate of 58 and HR 180. Pulse oximetry reading from the right upper extremity was 99%. The nose was not congested on exam but the patient had subcostal and tracheal retractions. He had a gallop on cardiac auscultation with clear lung auscultation and no hepatomegaly appreciated. His capillary refill was brisk. His femoral pulses were diminished though faintly palpable. On further examination, his pulse oximeter in his left leg was only 91%.
Diagnosis
The differential of tachypnea and increased work of breathing in the newborn is wide, but one of the most worrisome diagnoses is a ductal-dependent cardiac lesion. These lesions constitute “do-not-miss” diagnoses. While on initial history, this patient’s gradual tachypnea in the setting of a known close sick contact may have suggested an infectious etiology, his exam including diminished femoral pulses, lack of congestion, cardiac gallop, and asymmetric pulse oximeter readings between extremities was concerning for cardiogenic anomalies.
Discussion
Congenital heart disease is the most common birth defect in newborns and amounts to about 1% of all live births. [1] Critical congenital heart disease (CCHD) describes congenital cardiac defects that are life threatening and require operative intervention within the first year of life. CCHD accounts for 25% of congenital heart defects and is more common in males. [2] Of the cases of CCHD, 25% will be diagnosed after the newborn is discharged from the hospital, with variation in the type of CCHD. Of these, the most frequently missed defect is coarctation of the aorta. [3] One large study of 3746 live-born infants with non-syndromic CCHD from 1998-2007 noted that 62% cases of coarctation of the aorta were delayed in diagnosis. [4] Risk factors for delayed diagnosis of CCHD includes first born children, low maternal age, lack of family history of cardiac defects, and increased maternal pre-pregnancy BMI. [3]
Current screening for congenital heart disease includes fetal cardiac ultrasound in the second trimester with a four-chamber view of the heart as well as a view of the outflow tracts. However, this screening does not identify all congenital abnormalities. [3] One study found the highest predictor of prenatal diagnosis of congenital heart disease was maternal geographic location, suggesting access to care and technician skill may affect the sensitivity of this screening method. [3] A growing area of screening for CCHD that has more recently been recommended and adopted across the nation is pulse oximeter screening after 24 hours of life for newborns in well-infant and intermediate care nurseries, although it is still not yet standardized in every state or facility of the country. [5] In a review of 13 studies using pulse oximetry to screen for CCHD (single low pulse oximetry reading or discrepancy >3% between limbs), a sensitivity of 76.5% and a specificity of 99.9% was found, as well as a false-positive rate of only 0.05%. [2]
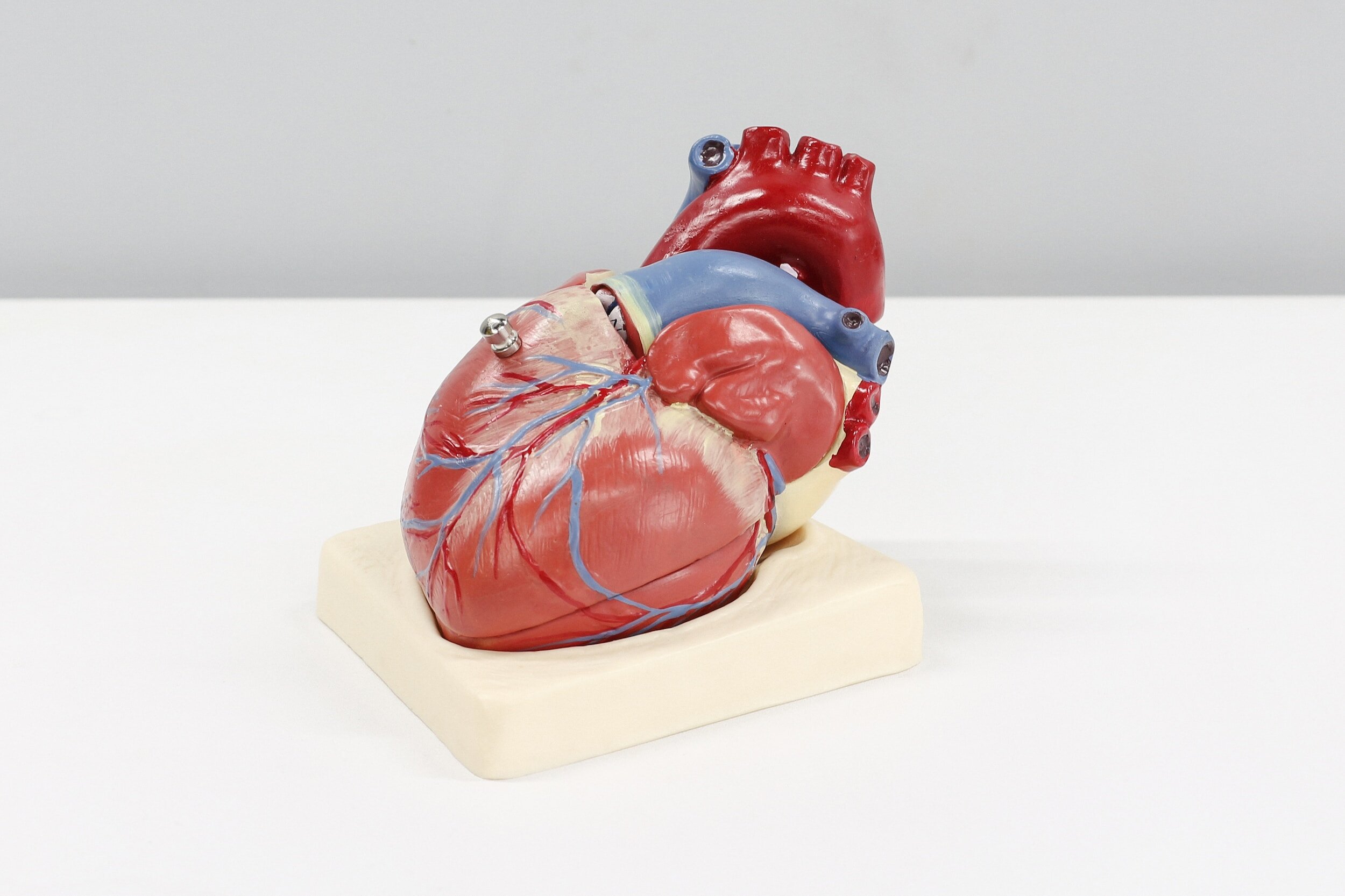
Image courtesy of Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities. [6]
While survival for infants with CCHD has significantly improved over time (67% over 1979-1993 to 82% over 1994-2005), prompt detection and referral to tertiary care centers is still crucial to the care of these patients. [2] In one study of newborns presenting to a tertiary care pediatric ICU with critical congenital heart disease, 60% presented initially with cyanosis and 74% with respiratory distress. [1] The differential diagnosis for these patients includes sepsis and endocrinopathy, and a careful history and exam, as well as early consultation with pediatric cardiologists is essential. The majority of critical congenital heart disease lesions rely on a patent ductus arteriosus (PDA), making prostaglandins the mainstay of treatment. [1] PDA dependent lesions can be grouped into three categories: restriction of pulmonary blood flow (pulmonary atresia, tricuspid atresia, and tetralogy of Fallot), restriction of systemic blood flow (coarctation of the aorta, hypoplastic left heart, severe aortic stenosis), and cardiac anomalies with mixing defects (transposition of the great vessels). [1] Administration of Prostaglandin PGE1 directly vasodilates the ductus arteriosus via smooth muscle relaxation and can reopen the ductus 30-120 minutes after administration. [1] The most life-threatening complication of PGE1 treatment, apnea, has been cited with a frequency of 16.7% in one study, and may be an indication for early intubation of these fragile patients prior to administration or prior to transport to a pediatric tertiary care center. [1]
Case Resolution
Broad laboratory studies, a viral panel, an electrocardiogram, and a chest x-ray were obtained. Notable results included an elevated lactate of 3.6 and sinus tachycardia on the electrocardiogram. Due to the concern for a cardiogenic cause of this patient’s presentation, pediatric cardiology was emergently consulted and performed a bedside echocardiogram which showed a large ventricular septal defect and severe coarctation of the aorta with closed ductus arteriosus. In discussion with the multidisciplinary pediatric cardiology team and ED team, the patient was initiated on prostaglandins, intubated for airway protection, and dispositioned to emergent surgical care and repair of his CCHD.
Take Aways
A careful history and exam are critical to evaluating for cardiogenic causes of neonatal critical illness in addition to infectious, metabolic, and endocrine etiologies.
Coarctation of the aorta is the critical congenital heart defect with the highest rate of diagnosis after discharge from the newborn nursery and most often presents with respiratory distress.
Pulse oximetry reading in multiple limbs is a validated screening tool although not yet universally adopted for detection of critical congenital heart disease.
Early consultation with a pediatric cardiologist in cases where a ductal dependent lesion is considered is critical to expediting treatment and coordination of resources for these high-risk patients.
Author: Katherine Stewart, MD, is a fourth-year emergency medicine resident at Brown Emergency Medicine Residency
Faculty Reviewer: Meghan Beucher, MD, is an Assistant Proferssor of Pediatrics and Emergency Medicine at Brown University
References
[1] Cucerea, M., Simon, M., Moldovan, E., Ungureanu, M., Marian, R., & Suciu, L. Congenital Heart Disease Requiring Maintenance of Ductus Arteriosus in Critically Ill Newborns Admitted at a Tertiary Neonatal Intensive Care Unit. Journal of Critical Care Medicine. 2016;2(4):185–191.
[2] Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics. 2013;131(5):e1502-e1508.
[3] Olney, R. S., Ailes, E. C., & Sontag, M. K. Detection of critical congenital heart defects: Review of contributions from prenatal and newborn screening. Seminars in Perinatology. 2015;39(3):230–237.
[4] Peterson C, Ailes E, Riehle-Colarusso T, et al. Late detection of critical congenital heart disease among US infants: estimation of the potential impact of proposed universal screening using pulse oximetry. JAMA Pediatr. 2014;168(4):361-370.
[5] Kemper AR, Mahle WT, Martin GR, et al. Strategies for implementing screening for critical congenital heart disease. Pediatrics. 2011;128(5):e1259-e1267.
[6] Congenital heart defects - facts about coarctation of the aorta. Centers for Disease Control and Prevention. February 2, 2023. Accessed November 7, 2023. https://www.cdc.gov/ncbddd/heartdefects/coarctationofaorta.html.