Forget About It: Diagnosis and Management of Transient Global Amnesia in the Emergency Department
“Transient global amnesia (TGA) is a period of sudden amnesia that involves the inability to recall recent memories as well as the inability to form new memories.”
Case
A 60-year-old female patient with a past medical history of anxiety presented to the emergency department (ED) with confusion. She remembered waking up in her usual state of health but did not remember the events that occurred during the morning and early afternoon. The patient’s daughter reported that the patient called her and said, “I feel so confused.” When family members went to check on the patient, they found her to be disoriented and asking repetitive questions. She denied any recent infectious symptoms, traumatic events, changes to her vision or speech, difficulty with ambulation, and any numbness or weakness.
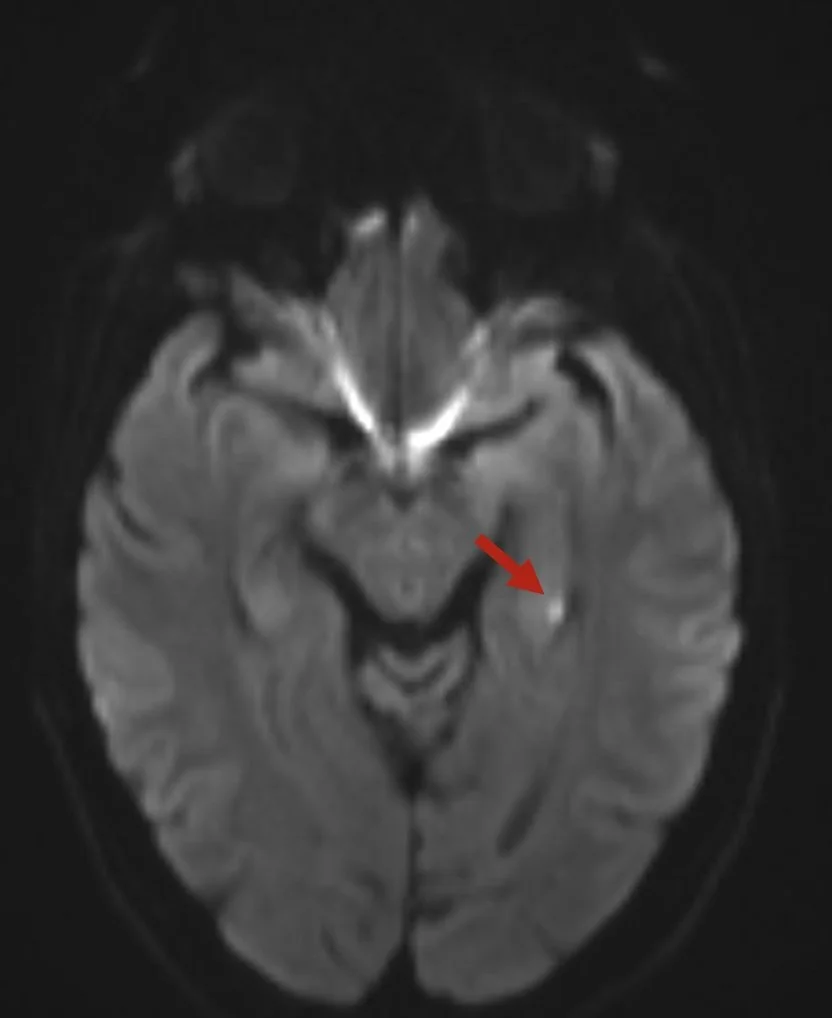
In the ED, vital signs were within normal limits. The patient was well-appearing, non-toxic, and alert. Neurologic examination including orientation, speech, cranial nerves, motor function, sensation, cerebellar testing, and gait was reassuringly normal. Upon leaving and reentering the room, however, the patient did not have any recollection of previous conversations with medical staff that occurred just several minutes prior. Blood work, urine drug screen, electrocardiogram, and non-contrasted computed tomography (CT) of the brain were unremarkable. As the patient’s short-term memory did not return to baseline, she was admitted for magnetic resonance imaging (MRI) of the brain which demonstrated a 3 mm area of restricted diffusion in the left medial temporal lobe.
Diagnosis
Transient Global Amnesia
Discussion
Transient global amnesia (TGA) is a period of sudden amnesia that involves the inability to recall recent memories as well as the inability to form new memories. [1] Symptoms usually last less than 24 hours and upon resolution, anterograde amnesia resolves. [1] TGA most frequently affects individuals between 50 and 70 years of age. [2] Several studies have demonstrated that patients with a history of migraine headaches may be at greater risk of developing TGA. [3,4] While the specific cause of TGA is unknown, up to 90% of cases include a precipitating event before symptom onset; these can include rapid temperature fluctuations, sexual intercourse, severe emotional/physical stress, pain, and medical procedures.[1,2] Pathogenesis of TGA involves the disruption of the neural connections that form memories, known as the Papez circuit.[1] Temporary interruption of these normal processes prevents access to and storage of short-term memories.[1]
Patients with TGA usually present to the ED with complaints of sudden onset of both retrograde and anterograde amnesia.[1] Patients may ask repetitive questions and will forget the answers after several minutes.[1] The remainder of the neurologic examination is otherwise unremarkable.[1] Patients must not present with other cognitive impairment, symptoms must not occur after head trauma or seizures, and symptoms should be expected to resolve within 24 hours.[1,2] When the diagnosis is uncertain due to an unclear history or confounding symptoms, CT, MRI, and electroencephalography can all be considered to rule out additional diagnoses.[1,2] Several studies have identified a correlation between TGA and the presence of abnormal, non-ischemic lesions in the left hippocampus or left medial temporal lobe seen on MRI diffuse-weighted imaging.[5-9] Figures 1 and 2 demonstrate representative images of these lesions. Ischemia, however, does represent a rare cause of isolated amnesia and some experts advocate for MRI evaluation for all patients with suspected TGA.[10]
There is no treatment for TGA, as symptoms will resolve without intervention.1 Patients should be observed until they have completely returned to their baseline.[1] Patients should be counseled that they will have a permanent gap in their memory equating to a period shortly before the event started until resolution of their anterograde amnesia.[1] Up to 30% of patients will have a recurrent episode of TGA.[1]
Case Resolution
The patient was seen by neurology who agreed with the diagnosis of TGA. Neurology, however, was concerned that the patient’s lesion seen on MRI could be ischemic in nature. The patient underwent CT with angiography of the brain and neck which did not show any abnormalities. Similarly, a transthoracic echocardiogram was also normal. The patient was started on daily aspirin, atorvastatin, and clopidogrel and was discharged with a plan to follow-up in the vascular neurology clinic. At the time of discharge, the patient’s memory had returned to baseline.
Take-Aways
TGA is a period of sudden amnesia that involves the inability to recall recent memories as well as the inability to form new memories.
Most cases of TGA are preceded by a physically or emotionally stressful trigger.
The diagnosis is clinical but advanced neuroimaging can be used to rule out alternative diagnoses.
MRI diffusion-weighted imaging can show left hippocampal/left medial temporal lobe lesions that are associated with TGA but not related to ischemia.
Symptoms usually resolve on their own within 24 hours.
Figure 1: An image from the case patient showed a punctate area of diffusion-restriction in the left medial temporal lobe seen on a magnetic resonance imaging diffusion-weighted imaging series.
Figure 2: An image from an additional patient showing a punctate area of diffusion-restriction in the left medial temporal lobe seen on a magnetic resonance imaging diffusion-weighted imaging series
Author: Jeffrey Savarino, MD, MPH, is a third-year emergency medicine resident at The Warren Alpert Medical School of Brown University.
Faculty Reviewer: Kristina McAteer, MD, is an Assistant Professor of Emergency Medicine and Clinical Educator at The Warren Alpert Medical School of Brown University. She is also an attending physician at Rhode Island Hospital and Newport Hospital.
References
1. Kirshner HS. Transient global amnesia: a brief review and update. Curr Neurol Neurosci Rep. 2011;11(6):578-82.
2. Bartsch T, Deuschl G. Transient global amnesia: functional anatomy and clinical implications. Lancet Neurol. 2010;9(2):205-14.
3. Lin KH, Chen YT, Fuh JL, Li SY, Chen TJ, Tang CH, Wang SJ. Migraine is associated with a higher risk of transient global amnesia: a nationwide cohort study. Eur J Neurol. 2014;21(5):718-24.
4. Liampas I, Siouras AS, Siokas V, Tsouris Z, Rikos D, Brotis A, Aloizou AM, Dastamani M, Dardiotis E. Migraine in transient global amnesia: a meta-analysis of observational studies. J Neurol. 2022;269(1):184-196.
5. Enzinger C, Thimary F, Kapeller P, Ropele S, Schmidt R, Ebner F, Fazekas F. Transient global amnesia: diffusion-weighted imaging lesions and cerebrovascular disease. Stroke. 2008;39(8):2219-25.
6. Strupp M, Brüning R, Wu RH, Deimling M, Reiser M, Brandt T. Diffusion-weighted MRI in transient global amnesia: elevated signal intensity in the left mesial temporal lobe in 7 of 10 patients. Ann Neurol. 1998;43(2):164-70.
7. Lee HY, Kim JH, Weon YC, Lee JS, Kim SY, Youn SW, Kim SH. Diffusion-weighted imaging in transient global amnesia exposes the CA1 region of the hippocampus. Neuroradiology. 2007;49(6):481-7.
8. Szabo K, Hoyer C, Caplan LR, Grassl R, Griebe M, Ebert A, Platten M, Gass A. Diffusion-weighted MRI in transient global amnesia and its diagnostic implications. Neurology. 2020;95(2):e206-e212.
9. Sparaco M, Pascarella R, Muccio CF, Zedde M. Forgetting the Unforgettable: Transient Global Amnesia Part II: A Clinical Road Map. J Clin Med. 2022;11(14):3940.
10. Michel P, Beaud V, Eskandari A, Maeder P, Demonet JF, Eskioglou E. Ischemic Amnesia: Causes and Outcome. Stroke. 2017;48(8):2270-2273.