Too Bad: Bi-mal Ankle Fractures
By Daniel Coleman, MD and Elizabeth Nestor, MD
CASE
A 62 year-old obese female with residual left-sided weakness from prior CVA presented with severe ankle pain after a fall. She was getting up from the toilet when her left knee gave out and she fell with her leg trapped underneath her body. After helping her back to bed, the patient’s daughter noticed her ankle and thought “it wasn’t supposed to look like that.”
Physical exam showed an obvious deformity of the left ankle, as well as skin tenting over the medial malleolus, but no open wound. The foot was neurovascularly intact, and the patient was able to move her toes. Her x-rays are below:
Figure 1. Tibiotalar joint dislocation and distal fibular fracture.
DIAGNOSIS
Tibiotalar joint dislocation and distal fibular fracture
DISCUSSION
Bimalleolar fractures
Ankle fractures have a variety of classification systems based on foot position and force, anatomy, and location of fracture. A bimalleolar fracture involves both the medial and lateral malleoli; a bimalleolar equivalent fracture involves the lateral malleolus, but there is also an associated deltoid ligament tear that results in lateral displacement of the talus, as with this patient. [1]
Physical exam
For any potentially broken ankle, assess for overlying wounds that may portend an open fracture, skin tenting, dislocation, associated tenderness in adjacent structures, pulses, sensation, and motor activity.
Imaging
A three-view of the ankle is a reasonable place to start, but external rotation stress radiographs have the highest sensitivity for deltoid ligament damage. Obviously, this view may be limited by pain or the ability to bear weight. If there is 5 mm of clear space between the lateral aspect of the talus and the medial aspect of the tibia, there is concern for damage of the deltoid ligament. [1]
Importantly, if there is any pulse, sensation, or motor deficit, reduction should be performed emergently. Injuries with skin tenting may also be reduced prior to imaging to prevent skin breakdown and development of an open fracture.
Pain control
Ankle fracture/dislocations require robust pain control with narcotic pain medications. Some patients may also benefit from the muscle-relaxing activity of a benzodiazepine. In this case, the patient experienced muscle spasms of the affected leg, which responded to a small dose of Ativan, enabling efficient reduction of the ankle. Ice and elevation are useful adjuncts, and will also reduce swelling.
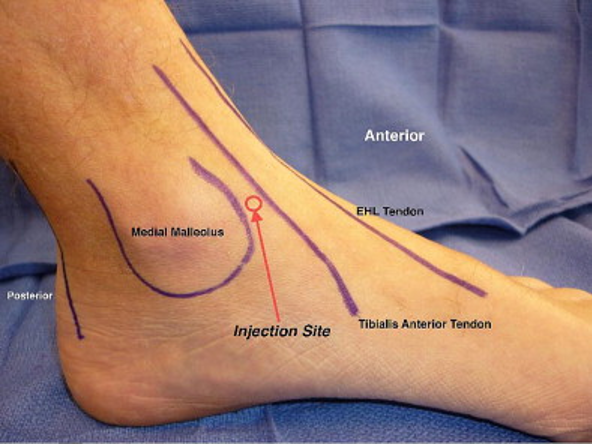
Prior to reduction, a hematoma block with 10 mL of 1% lidocaine into the ankle mortise will provide effective local anesthesia. To find the mortise for your hematoma block, palpate the tendon of the tibialis anterior, aspirate blood medial to the tendon, and then inject at the level of the medial malleolus. (Figure 2)
Figure 2. Ankle anatomy for hematoma block. [2]
Reduction
Reduction typically requires two people. One will hold the hip and knee in 90 degrees of flexion to provide counter traction and take tension off the gastrocnemius. The other person places one hand on the heel and another on the dorsum of the foot. Initially, recreate the injury to disengage the bone, after which the foot is pulled distally into alignment. After reduction, the foot must be maintained in supination by holding the toes to maintain the reduction. [3]
Figure 3. Reduction technique for ankle fracture. [3]
If a second person is not available to assist with the reduction, you may sit the patient on the edge of the bed, high enough so their foot does not touch the floor. This position gives you the appropriate 90 degrees of flexion. From here, the technique for reduction is similar to that described above, except the overall vector is down.
Splinting
Stabilize the ankle with a posterior splint and stirrups. Be sure to have your splinting materials cut to length and readily available. After reduction, an assistant must hold the foot to maintain the reduction while the split is applied.
Operative fixation
Unless the patient is elderly, has non-weightbearing status at baseline, or would not tolerate surgery, operative fixation is the definitive treatment for bimalleolar equivalent fractures. It is not necessary to repair the medial deltoid ligament, and repair of the lateral malleolus is typically accomplished via plating.
CASE RESOLUTION
Correct alignment of the patient’s ankle was accomplished after reduction in the emergency department. The patient was admitted to the orthopedics service for eventual operative fixation and discharged to short-term rehab.
TAKE-AWAYS
Five milimeters of clear space between the lateral aspect of the talus and the medial aspect of the tibia is concerning for damage of the deltoid ligament and medial malleolar fracture.
For any pulse, sensation, or motor deficit, or significant skin tenting, reduction should be performed emergently.
Reduction is typically a two-person job, but may be attempted by a single practitioner, if necessary. Pain control and muscle relaxation are essential.
Authors:
Daniel Coleman is a fourth-year Emergency Medicine Resident at Brown University
Elizabeth Nestor is a Clinical Professor of Emergency Medicine at Brown University
REFERENCES
Taylor B. Ankle Fractures. OrthoBullets. https://www.orthobullets.com/trauma/1047/ankle-fractures. Accessed January 15, 2018.
Ross A, Catanzariti A, Mendicino R. The Hematoma Block: A Simple, Effective Technique for Closed Reduction of Ankle Fracture Dislocations. J Foot Ankle Surg. 2011; 50(4): 507-509.
Roman SR. Closed Reduction of Displaced Ankle Fractures. The Podiatry Institute: Update, 2005.