Open Extensor Tendon Repair in the ED
CASE
Your patient is a 25-year-old male with a right hand laceration presenting the day after a “fight.” The patient says that he doesn’t remember what happened because he and his friends were drinking but thinks that he might have gotten into a fight the preceding night.
On exam, his right 4th finger is flexed at the metacarpophalangeal (MCP) joint and neutral at the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints and he has a 2 cm laceration over the 4th and part of the 5th MCP joint of his right hand. Sensation is intact and the distal tips of the fingers have good capillary refill. He is unable to extend his 4th digit at the MCP joint and has weak extension of the PIP and DIP. On deeper examination of the wound while ranging the joints, you note that the extensor tendon is severed.
Because you are super-classy, you say: “Whelp, gotta hand it to you; you really messed up.”
DIAGNOSIS
Open right 4th extensor tendon laceration
DISCUSSION
Background:
Epidemiologically, patients with this type of injury will tend to be males, with their dominant hand injured. The thumb is the most commonly injured digit, followed by the middle finger, and most injuries occur at or distal to the MCP joint. The most common mechanism is with sharp laceration but injuries due to saws or other power tools are associated with bone and soft tissue damage around half of the time. [1] This post deals with uncomplicated laceration-type extensor tendon injuries without bone or joint involvement.
Anatomy:
It’s time to harken back to our STEP 1 days and review the anatomy/physiology of the dorsum of the hand. [2] There are — as grandma might say — “a whole bunch” of bones, vasculature, nerves, and muscles which move the hand. However, many of these structures lie either high up on the forearm or on the palmar aspect of the hand and are protected from such injuries. Unfortunately the tendons tend to get injured on the back of the hand because there is little protective tissue and sparse overlying fat.
The nerves of the hand are easily arranged by division into sensory and motor nerves. In the case of the back, or dorsum, of the hand almost all of the sensation is provided by the radial nerve with the ulnar nerve providing the sensation to the 4th and 5th digits. The radial nerve also provides motor functions to the extensor muscles of the wrist, and any muscles of the dorsum of the hand which originate in the forearm. The ulnar nerve provides the motor function to the 4th and 5th intrinsic hand muscles, or lumbricals, with the median nerve providing motor function to the 2nd and 3rd lumbricals.
Due to the insertions of the different muscles and various tendons, different muscles move different finger joints. The DIPs are moved by the lumbrical muscles because the insertion of the lumbrical insertion is located near the distal tuft on the extensor expansion. The PIPs are moved by both the lumbrical muscles and the extensor digitorum. The MCPs are extended by the extensor digitorum because the tendon inserts just distal to the PIP on the extensor expansion.
All of this together explains why a good physical exam is critical prior to final disposition of patients with hand injuries. Even though lacerations to the dorsum may not appear deep, it is likely to involve the extensor tendon, and other examination findings should clue you in to other more sinister pathology.
Figure 1 LUMBRICAL MUSCLE ACTION, [2] Netter’s Concise Orthopaedic Anatomy.
Repairs:
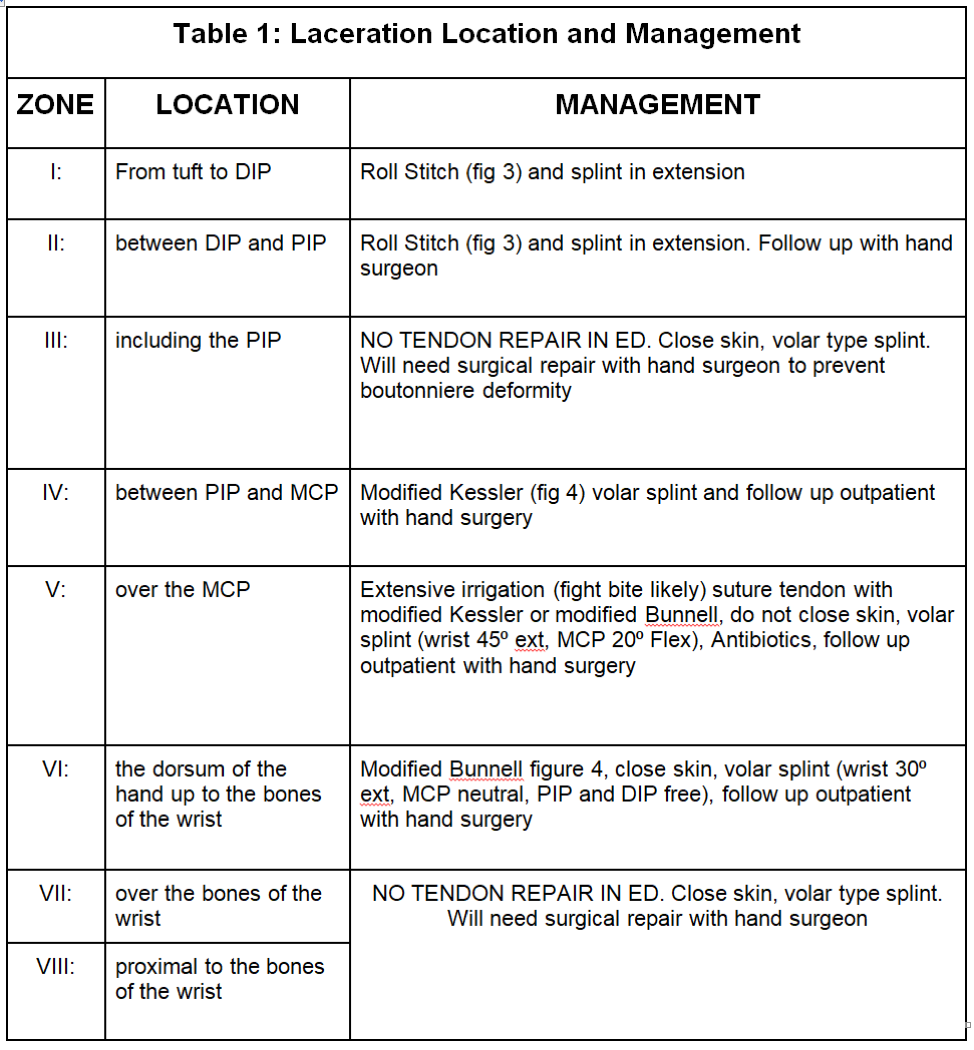
Once you have a handle on the anatomy, the repair/management of extensor tendons is guided by location and the severity of injury. The dorsum of the hand can be broken down into 7 zones.
Figure 2 EXTENSOR ZONES OF THE HAND, [2] Netter’s Concise Orthopaedic Anatomy.
In most zones, simple lacerations of the extensor tendons can be repaired in the emergency department because the tendon is superficial which means that the vital structures are protected on the palmar side of the hand.
Tendon injury in Zones I and II can be stitched [figure 3] and splinted in extension. Zone IV can be repaired with a modified Kessler stitch and splinted with a volar splint. Zone V — as in our patient — should be extensively irrigated for concerns of fight bite. It should then be repaired with either a modified Kessler or Bunnell stitch and left open. Splint with the wrist at 45⁰ of extension, and the MCP at 20⁰ of flexion, and provide urgent follow up with hand surgery. Zone VI is also repaired with Bunnell stitch and splinted with the wrist at 30⁰ and the MCP neutral.
Essentially, all tendon injuries will need outpatient follow up with a hand surgeon. Theoretically isolated zone I injury with no risk factors and good follow up could be referred to a PCP, but in practice a referral should be placed.
Some zones, such as Zone III, VII and VIII have challenges to repair which require an expertise beyond the scope of the emergency department. Zone III involves the complex interaction of the lumbrical insertion, the extensor insertion and the extensor expansion. Zones VII and VIII have musculature, extensor tendon sheaths and other potential anatomic complications.
Figure 3 Roll Stitch [8]
Figure 4: Suture Types for Tendon Repair. [6]
CASE RESOLUTION
After extensive irrigation our patient’s tendon was repaired, the wound was packed with iodoform and left open, the hand was splinted in extension with the MCP in mild flexion, and he was given amoxicillin and clavulanate 875/125 twice daily for 5 days and instructed to follow up with hand surgery to schedule his operation within the week.
TAKE-AWAYS
Many extensor tendon injuries can be repaired in the ED.
Antibiotics should be administered if the wound is dirty (fight bites) or if it requires delayed closure and follow-up.
Consider tendon repair in resource limited environments or in community settings.
Do not perform ED repair for lacerations in zone III (over the PIP) or at/proximal to the wrist
You did it. Nice job; give yourself a hand.
AUTHOR: Russell Prichard MD is a 3rd year Emergency Medicine Resident for Brown University
FACULTY REVIEWER: Shideh Shafie MD, Assistant Professor of Emergency Medicine Brown Universtiy
REFERENCES
Patillo D, Rayan G. Open extensor tendon injuries: an epidemiologic study. Hand Surgery: An International Journal Devoted To Hand And Upper Limb Surgery And Related Research: Journal Of The Asia-Pacific Federation Of Societies For Surgery Of The Hand [serial online]. 2012;17(1):37-42. Available from: MEDLINE, Ipswich, MA. Accessed September 15, 2018.
Thompson, Jon C. Netter’s Concise Orthopaedic Anatomy, CHAPTER 6, 183-218
Griffin M, Hindocha S, Jordan D, Saleh M, Khan W. Management of Extensor Tendon Injuries. The Open Orthopaedics Journal. 2012;6:36-42. doi:10.2174/1874325001206010036.
Extensor Tendon Repair [Internet]. Medscape. 2021 [accessed 2021 April 2] available from https://emedicine.medscape.com/article/109111-overview
Extensor Tendon Injuries [Internet]. Orthobullets. 2021 [accessed 2021 April 2] available from https://www.orthobullets.com/hand/6028/extensor-tendon-injuries
Extensor and Flexor Tendon Injuries in the Hand, Wrist, and Foot [Internet]. Veterian Key 2016 [accessed 2021 April 2] available from Extensor and Flexor Tendon Injuries in the Hand, Wrist, and Foot | Veterian Key
McBrien B. Fight bite injury: emergency department assessment and management. Emergency Nurse [serial online]. November 2016;24(7):34-37. Available from: Academic Search Premier, Ipswich, MA. Accessed September 15, 2018.
Emergency Department Management of Extensor Tendon Lacerations [Internet]. ACEPNow. 2015 [accessed 2021 April 2] available from Emergency Department Management of Extensor Tendon Lacerations - Page 3 of 4 - ACEP Now | Page 3
![Figure 1 LUMBRICAL MUSCLE ACTION, [2] Netter’s Concise Orthopaedic Anatomy.](https://images.squarespace-cdn.com/content/v1/56e8a86a746fb97ea9d14740/1617669444986-UV26ZW63KMASN36UE3BS/lumbrical.png)
![Figure 2 EXTENSOR ZONES OF THE HAND, [2] Netter’s Concise Orthopaedic Anatomy. ](https://images.squarespace-cdn.com/content/v1/56e8a86a746fb97ea9d14740/1617669482432-DTATBXMIJK64COEBNSWL/extensor.png)
![Figure 3 Roll Stitch [8]](https://images.squarespace-cdn.com/content/v1/56e8a86a746fb97ea9d14740/1617669516663-W4AETR1AVVZ5WV8RCHKC/roll+stitch.png)
![Figure 4: Suture Types for Tendon Repair. [6]](https://images.squarespace-cdn.com/content/v1/56e8a86a746fb97ea9d14740/1617669549398-Q9MHOZ3MN4QXUF2NLWEI/tendon+repair.png)