Volume Assessment Using POCUS in the Emergency Department
CASE
An 83-year-old male with a history of HFrEF (40%), CAD, hypertension, and hyperlipidemia presented to the ED with generalized weakness and fatigue. His vitals were remarkable for hypotension with a MAP of 58. On physical exam, the patient appeared non-toxic and was able to answer questions appropriately. He did not appear frankly fluid overloaded, other than mild, chronic peripheral edema. Additional laboratory studies and chest x-ray were performed. A fluid bolus was given to treat his hypotension, however there was minimal response. Given his heart failure, there was concern that aggressive fluid resuscitation would result in pulmonary edema. Additionally, inserting a central line and starting vasopressors is not without risk. Fortunately, this clinical team knows how to use ultrasound to do a proper volume assessment to manage this patient appropriately.
DIAGNOSIS
Traditional Methods of Volume Assessment
As we all know, it can be challenging to know where a patient lies on the Starling curve, leading to uncertainties surrounding adequate resuscitation in shock. Although it seems benign, sometimes too much fluid can be quite dangerous for a patient. Increasing intravascular volume in a patient who is already overloaded can push a patient off the Starling curve, causing pulmonary edema and respiratory distress.
Classically, critical care physicians have used CVP measurement and pulmonary artery occlusion pressure, however, these methods are invasive and do a poor job of predicting fluid responsiveness. Stroke volume measurements can also be useful in certain situations; however, this is easiest to achieve in a fully mechanically vented patient. Overall, these measurements have limited use to the emergency physician.[1]
Some other ways to assess a patient’s volume status in the ED includes the passive leg raise (PLR) and small bolus fluid challenges.
To perform a PLR the provider lifts the legs of a patient from a horizontal supine position. This technique induces a mobilization of intravascular volume from the lower extremities towards the heart. PLR redistributes 300–500 mL of intravascular volume to the heart. Overall, PLR is an easily performed, non-invasive way to assess fluid responsiveness.[2]
Figure 1. Proper positioning for a passive leg raise.[3]
POCUS: IVC Assessment
In the ED point-of-care ultrasound (POCUS) is a vital component of patient diagnosis for many conditions and is used for procedural guidance. Using POCUS in the evaluation of hemodynamically unstable patients is crucial both for diagnosing the cause of shock, and for assessing fluid status. Evaluation of the IVC can be helpful in the emergency department setting. Providers can assess whether the IVC is “plethoric” or “kissing”, and how much collapse occurs with the IVC during respiration (caval index).
To obtain a view of the IVC, place a high penetration, low frequency probe (such as the phased array or curvilinear probe) in the subxiphoid space in the sagittal plane, with the probe-marker towards the patient’s head. Once you find the IVC, you may need to rock your probe in a slight cranial position to observe it emptying into the right atrium. Make sure you are interrogating the IVC and not the aorta (the IVC will be on the right side of the patient’s body compared to the aorta).[4]
Figure 2. Proper probe positioning for IVC assessment [4]
Once this view has been obtained, the clinician can begin to assess volume status by asking the patient to breath normally, observing for collapsibility. The best place to assess the collapsibility is 2cm from the RA/IVC junction. The calculation for collapsibility index is:
[(IVC Diameter Max – IVC Diameter Min)/IVC Diameter Max] X100
Figure 3. Examples of a flat or “kissing” IVC (left) and a “plethoric” IVC (right) during inspiration. [5]
If the IVC is <1cm and/or collapses >75%, the patient is likely volume depleted (sepsis, bleeding, dehydration, etc) and may be able to tolerate more fluids. If the IVC is >2cm and has minimal collapsibility (cardiogenic or obstructive shock), the patient may be less likely to tolerate aggressive fluid resuscitation. Patients taking exaggerated, deep breaths will have more respiratory variation in their IVC, so it is important to ask patients to breath normally during this assessment. Mechanical ventilation and elevated right heart pressures will impact the accuracy of IVC assessment.[6]
Using IVC as an assessment of volume status is not always perfect. There is variability among ultrasound users however, studies demonstrate moderate reliability of IVC measurement between emergency medicine residents of different post-graduate years.[7] There can also be challenges with obtaining a clear view of the IVC in obese patients or patients with bowel gas overlying the IVC. Overall, assessment of the IVC using POCUS provides valuable information regarding volume status, especially in the proper clinical setting.
Measuring Carotid Flow Time with POCUS
Another way to use POCUS to evaluate volume status is to assess the carotid blood flow and flow time.
The technique involves measuring the flow through the carotid artery before and after straight leg raise. If there is an increase of >10% of flow time, then the patient is likely to respond well to fluid resuscitation.[8]
The following video from the ultrasound team at MGH is quite useful in explaining how to obtain and interpret this data: https://www.youtube.com/watch?v=YRFweWHCjsQ 9
Obtaining Carotid Flow Time:
1) Find the common carotid artery (CCA) in a transverse view with a linear probe
2) Rotate the probe 90 degrees and center the common carotid artery in a longitudinal plane
3) Slide the probe up the vessel until the carotid bulb is seen. Measurements will be taken just distal to this location (Figure 4)[9]
Figure 4. Identification of the Carotid Bulb
4) Place the pulse wave doppler gate in the center of the vessel. Ensure that the correction angle is parallel to the carotid artery and that the angle of the gate and the steering line is less than 60 degrees. (Figure 5)[9]
Figure 5. Measuring Carotid Flow
5) Obtain pulse wave doppler images
6) Obtain systole time which is from the start of systole to the start of the dicrotic notch (Figure 6)[9]
Figure 6. Pulse Doppler Images
7) Then obtain cycle time, which is the start of systole to the end of the cycle (Figure 7)[9]
Figure 7. Cycle Time
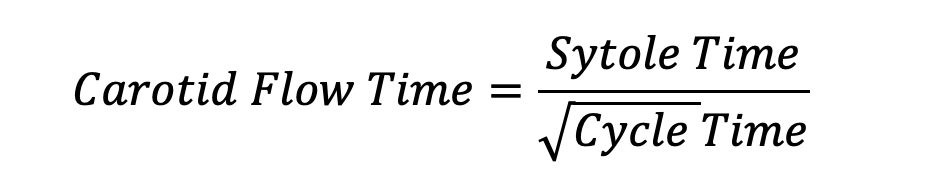
8) You can then use these variables to calculate flow time with the following equation:
This process can be repeated when the patient is in a PLR position to determine if they are fluid responsive. One study demonstrated a specificity of 96%, sensitivity of 68%, positive predictive value of 97% and 82% accuracy in corrected carotid flow time successfully predicting fluid responsiveness.[10] However, other studies have shown that reproducibility of data among users is poor, and Flow Time may not be the most useful method in assessing volume status.[11]
Ultimately, neither IVC ultrasound nor corrected carotid flow time are perfect measures in determining response to fluid resuscitation. They are certainly valuable pieces of information that can be used within the overall clinical context of a patient presentation to determine the best course of action in treatment of hypotension.
TAKE-AWAYS
Volume assessment in hypotensive patients is critical to providing proper treatment.
POCUS is a valuable tool for volume assessment in the critically ill.
IVC measurement is best done in patients who are not mechanically ventilated with normal inspiratory effort. An IVC <1cm with significant respiratory variation can indicate a patient is fluid down, whereas an IVC which is plethoric with limited respiratory variation may be a sign of cardiogenic or obstructive shock causing hypotension.
Carotid Flow time is another POCUS method to assess volume status before and after passive leg raise. If the carotid flow time increases by 10%, the patient may respond well to fluid resuscitation.
It is critical to use POCUS within the clinical context of the patient to provide excellent care to critically ill patients.
AUTHOR: Joshua Nims, MD, is a current second year emergency medicine resident at Rhode Island Hospital/Brown University.
FACULTY REVIEWER: Kristin Dwyer, MD
REFERENCES
Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008 Jul;134(1):172-8. doi: 10.1378/chest.07-2331. PMID: 18628220.
Pourmand A, Pyle M, Yamane D, Sumon K, Frasure SE. The utility of point-of-care ultrasound in the assessment of volume status in acute and critically ill patients. World J Emerg Med. 2019;10(4):232-238. doi:10.5847/wjem.j.1920-8642.2019.04.007
Misango D, Pattnaik R, Baker T, et al. Hemodynamic Assessment and Support in Sepsis and Septic Shock in Resource-Limited Settings. 2019
Inferior Vena Cava POCUS: The Basics of Image Acquisition. The Renal Fellow Network: https://www.renalfellow.org/2020/03/20/inferior-vena-cava-pocus-the-basics-of-image-acquisition/
WikEM: IVC Ultrasound – Clips: https://wikem.org/wiki/IVC_ultrasound
Akkaya A, Yesilaras M, Aksay E, Sever M, Atilla OD. The interrater reliability of ultrasound imaging of the inferior vena cava performed by emergency residents. Am J Emerg Med. 2013 Oct;31(10):1509-11. doi: 10.1016/j.ajem.2013.07.006. Epub 2013 Sep 5. PMID: 24012423.
Ma IWY, Caplin JD, Azad A, et al. Correlation of carotid blood flow and corrected carotid flow time with invasive cardiac output measurements. Crit Ultrasound J. 2017;9(1):10. doi:10.1186/s13089-017-0065-0
MGH Ultrasound: https://www.youtube.com/watch?v=YRFweWHCjsQ
Barjaktarevic I, Toppen WE, Hu S, et al. Ultrasound Assessment of the Change in Carotid Corrected Flow Time in Fluid Responsiveness in Undifferentiated Shock. Crit Care Med. 2018;46(11):e1040-e1046. doi:10.1097/CCM.0000000000003356
Doctor M, Siadecki SD, Cooper D Jr, Rose G, Drake AB, Ku M, Suprun M, Saul T. Reliability, Laterality and the Effect of Respiration on the Measured Corrected Flow Time of the Carotid Arteries. J Emerg Med. 2017 Jul;53(1):91-97. doi: 10.1016/j.jemermed.2017.01.056. Epub 2017 Mar 25. PMID: 28351511.