Recognizing the Differential Diagnoses for Erythema Multiforme
CASE
This is a 4-year-old female with a chief complaint of 2 days of rash. She appears to be completely unbothered by the rash, and has been afebrile without any recent infections/illnesses. A complete review of systems is negative. The patient has been eating and drinking well and her behavior is at baseline. Her mother at bedside denies any new exposures such as detergent, lotion, and food. She has no significant past medical history and does not take any medications; she is up to date on vaccines and has not received any new vaccines recently. Vital signs are within normal limits for age. The physical exam is significant for diffusely scattered, erythematous “targetoid” lesions along with equally scattered erythematous, slightly raised wheals. This rash is found on her trunk, extremities, and palms. There is no mucosal involvement.
Figure 1. Diffuse “targetoid” lesions
DIAGNOSIS
Urticaria Multiforme
DISCUSSION
The initial assessment of this patient’s rash was erythema multiforme given the classic “target” appearance of the lesions. However, upon repeat examination of the rash with the attending physician, the presence of the wheals added urticaria multiforme to the differential diagnosis. This diagnosis was confirmed after giving the patient a dose of Benadryl, which caused the rash to become less erythematous and less raised.
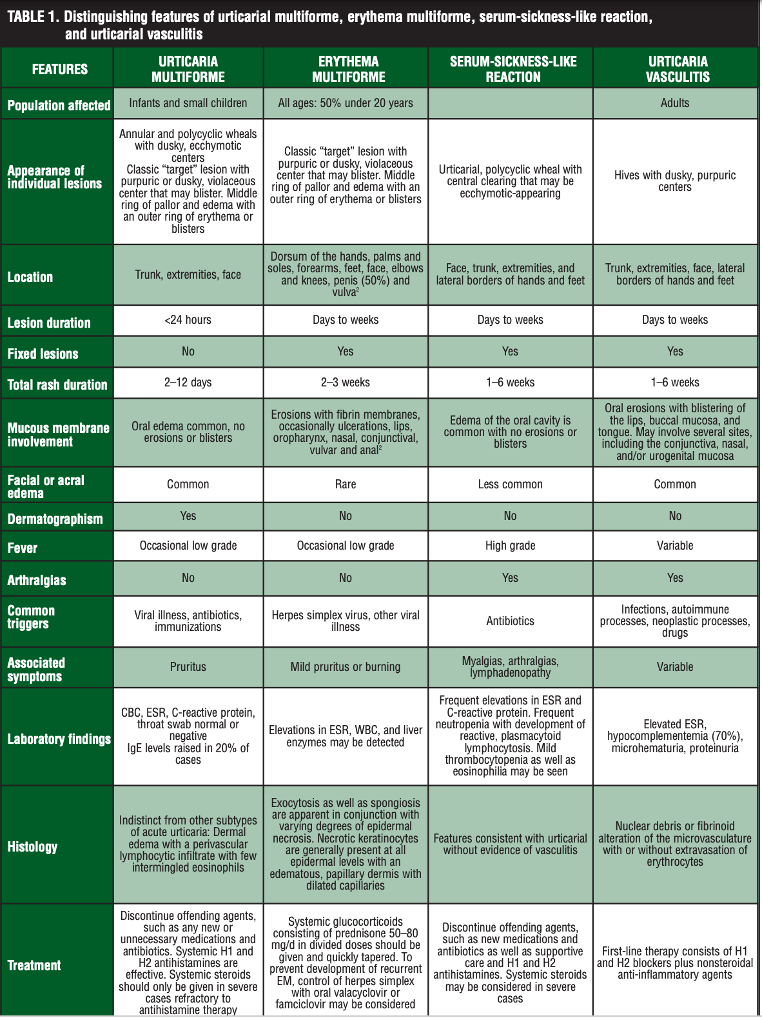
“Urticaria multiforme is a benign cutaneous hypersensitivity reaction seen in pediatric patients that is characterized by the acute and transient onset of blanchable, annular, polycyclic, erythematous wheals with dusky, ecchymotic centers in association with acral edema. It is most commonly misdiagnosed as erythema multiforme” [1]. The differential diagnosis for erythema multiforme includes urticarial multiforme, erythema multiforme, serum-sickness-like reaction, and urticarial vasculitis, among others. While all of these rashes may appear similar on exam, distinguishing between them is imperative given that the diagnosis determines management, as shown in Table 1 below.
Table 1. Distinguishing between urticarial multiforme, erythema multiforme, serum-sickness-like reaction, and urticarial vasculitis [1]
In all rashes, the history and physical exam are critical to reaching a diagnosis. Although a serum-sickness like reaction is on the differential for this patient’s rash, this diagnosis was unlikely without any fever, lymphadenopathy, or joint pain and swelling. Urticaria vasculitis was lower on the differential given the rash started just two days ago and there was no mucus membrane involvement. Understanding that erythema multiforme is associated with an infection 90% of the time makes this diagnosis less likely for this patient who did not have any history of recent illness [2]. An interesting method to help make the distinction between erythema and uriticarial multiforme is to look for dermatographism, where the provider writes on the patient and then looks for raised wheals on the skin as a response to that trauma. “Dermatographism secondary to mast cell mediated cutaneous dermal hypersensitivity at sites of skin trauma is a common part of the clinical picture in affected patients that can manifest in geometric or linear patterns” [1].
Figure 2. Dermatographism [1]
In the literature, there exists a collection of case reports on the dermatologic manifestations of COVID-19. One of these case reports describes an 18-year-old who presented with “disseminated, asymptomatic and not evanescent annular erythematous urticarial papules and plaques, some with targetoid appearance…” with sparing of the mucosa [1]. This rash is consistent with urticarial multiforme. The patient did not have any other symptoms and was found to have COVID-19. The case was published to bring attention to skin manifestations as a possible first presenting symptom of early COVID-19 infection.
The treatment of urticaria multiforme with oral antihistamines is largely for symptom management given the rash will self-resolve in 2-10 days. Administering the first dose of antihistamine while in the emergency department, and watching for improvement in the rash’s appearance, can help to definitively make this diagnosis.
CASE RESOLUTION
Patient was discharged with a prescription for oral Benadryl and close primary care follow up.
TAKE-AWAYS
· The presence of wheals amongst “targetoid” lesions should raise suspicion for urticarial multiforme
· Dermatographism is a unique tool that can help identify rashes mediated by hypersensitivity
· Improvement after antihistamine administration can help to distinguish urticaria multiforme from erythema multiforme
Author: Kaitlin Lipner, MD is a second-year resident at Brown University/Rhode Island Hospital
Faculty Reviewer: Jane Preotle, MD
REFERENCES
1. Emer JJ, Bernardo SG, Kovalerchik O, Ahmad M. Urticaria Multiforme. Clinical Aesthetic Dermatology. 2013;6(3):34-39.
2. Trayes KP, Love G, Studdiford JS. Erythema Multiforme: Recognition and Management. American Family Physician. July 2019:82-88.
3. Mendes CC, Pimenta R. Urticaria multiforme-like: A COVID-19 infection. Pan African Medical Journal. 2020;37. doi:10.11604/pamj.2020.37.286.26740
4. Starnes L, Patel T, Skinner RB. Urticaria multiforme-a case report. Pediatric Dermatology. 2011;28(4):436-438. doi:10.1111/j.1525-1470.2011.01311.x