Obstructive Hydrocephalus Due to Intraventricular Neurocystircercosis
…gradual onset headache was accompanied by vomiting, subjective fevers, intermittent dizziness and generalized weakness…
case
A 21-year-old Spanish-speaking gentleman presented to the emergency department with the chief complaint of abdominal pain. It quickly became apparent that the abdominal pain was not his chief concern and he was most bothered by three days of waxing and waning headache. The evaluation was complicated by the patient’s significant anxiety, making obtaining a history difficult despite the use of a video interpreter.
He reported three days of a gradual onset headache that was accompanied by vomiting, subjective fevers, intermittent dizziness and generalized weakness. A family member accompanied the patient and described the patient being "loose" when walking down the stairs, and needing help to do so. This observation by family prompted the emergency department (ED) visit.
After arrival to the ED the patient noticed weakness of his right arm and leg and as did spasms of both hands. The patient was quickly brought back to a treatment room and seen by a physician within 20 minutes of presentation
The patient had no relevant past medical history or family history. He took no medications and had no allergies. He was an immigrant from Guatemala and had resided in the US for 2 years.
In the emergency department, the patient was anxious and hyperventilating. He had a blood pressure of 109/52 mmHg, heart rate of 120 beats per minute, oral temperature of 98 degrees Fahrenheit, respiratory rate of 19 breaths per minute and oxygen saturation of 100% on room air.
On physical exam, he was tachycardic and anxious. The remainder of his cardiopulmonary exam was unremarkable. His neurologic exam was significant for 4 out of 5 strength in the right upper extremity and the right lower extremity, 4 out of 5 grasp on the right and drift of both right upper and right lower extremity. He had dysmetria on right upper and lower extremity testing, as well as ataxic gait.
As the patient had an acute neurologic deficit, a computed tomography (CT) as well as a computed tomography angiography (CTA) of the head and neck were emergently performed. The non contrast CT demonstrated markedly dilated fourth ventricle, with mild dilatation of the third and lateral ventricles. This was consistent with likely obstructive hydrocephalus.
The patient was transferred to the regional tertiary care center, and subsequently an magnetic resonance imaging (MRI) of the brain demonstrated a partially collapsed, non-enhancing "cyst" obstructing the foramena of Magendie.
diagnosis
Obstructive hydrocephalus due to intraventricular neurocystircercosis.
discussion
BACKGROUND
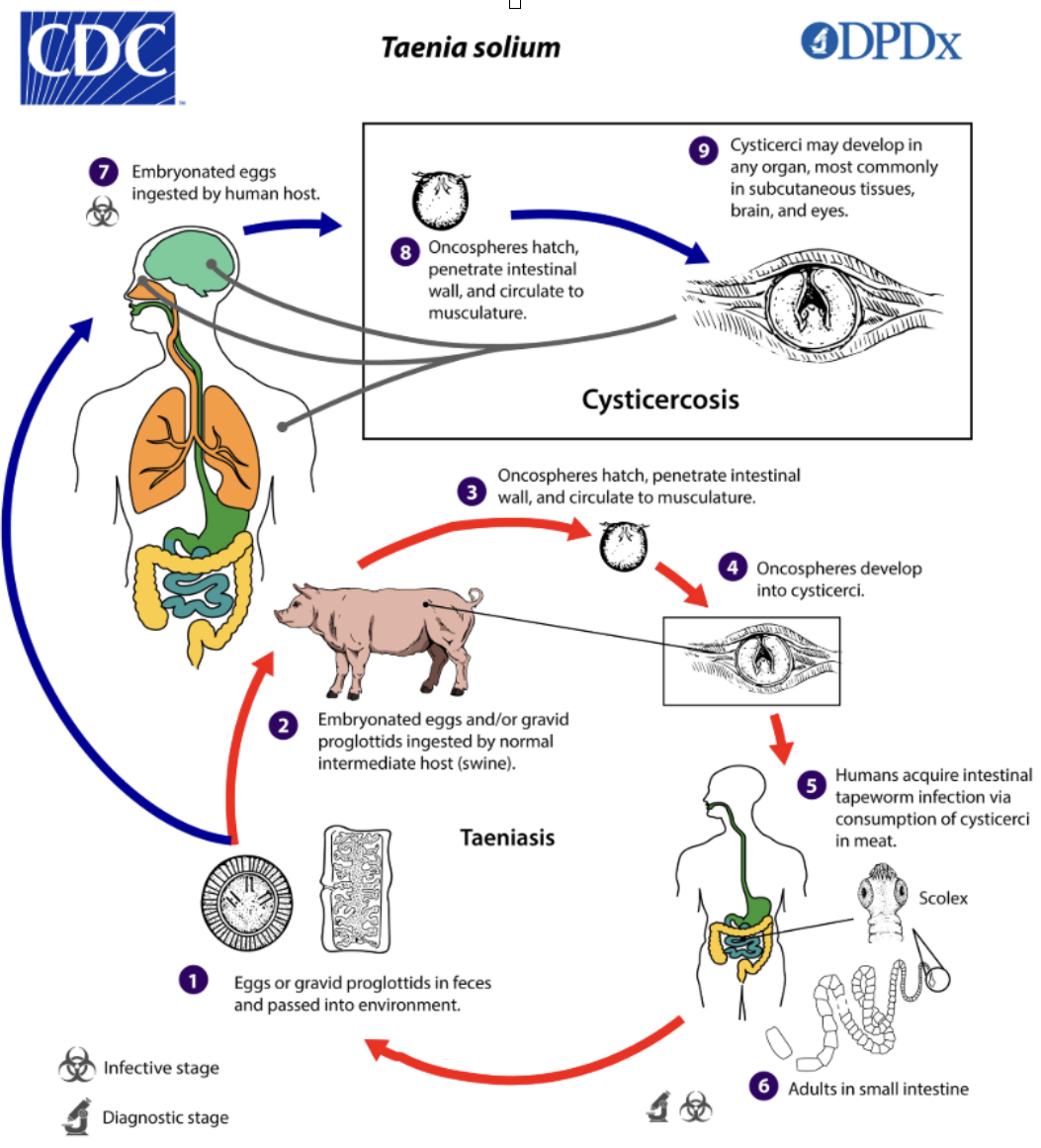
Cysticercosis is an infection by the pork tapeworm, Tania solium. Though infection is possible in multiple tissues, it is most common in the subcutaneous tissue, brain and eyes. Neurocysticercosis is the most morbid manifestation of the disease and occurs when the larval stage of the parasite, known as cysticerci, invade the central nervous system. Most cysts outside the central nervous system are asymptomatic. An estimated 50,000 deaths per year are attributed to neurocysticercosis, making this disease the leading cause of death from food borne illness.
Tenia solium is endemic in Mexico, Central and South America, Southeast Asia and Africa. Swine and humans are the host species. Ingestion of undercooked pork infected with cysts results in taeniasis, a human carrier state for the pork tapeworm. Cystircesosis occurs via fecal oral transmission, including via auto transmission in cases of taeniasis, after ingestion of T solium eggs. Humans are the only known definitive host for T solium, and the tapeworm is able to produce eggs only while residing in the human intestine. Once ingested, oncospheres hatch from tapeworm eggs in the digestive system of the human host, thereafter penetrating the intestinal mucosal and entering the blood stream. From there they travel to distant tissue sites, including the CNS. Though cysts often are destroyed by our immune system, those deposited inside the blood brain barrier may evade this fate and remain within the CNS for years, resulting in neurocysticercosis. (Image 1)
Surviving T solium form cysts evading the immune response, and a lesion without surrounding inflammation forms. This results in a a scolex (parasite head) within a membrane bound cyst. The parasite can persist in this state for years, until it begins to degenerate and a surrounding inflammatory response develops, often resulting in symptoms. Gradually the cyst further degenerates and the scolex deteriorates, eventually collapsing into a small granulomatous lesion. Over time either the necrotic parasite is resorbed, or a calcified scar develops.
Image 1. Transmission & life cycle of Taenia Solium [Source: CDC]
CLASSIFICATION
Neurocysticerosis is classified based on location of lesions. In parenchymal disease lesions most often form at the gray/white interface, and are often symptomatic due to seizures, headaches, or mass effect. Extraparenchymal neurocysticercosis can occur in the subarachnoid space, ventricular space, within the spinal cord or spinal subarachnoid space, or within the eye. Symptomatology is variable but depends on the location and number of the cysts. Subarachnoid disease can result in stroke and vasculitis, mass effect and inflammation, optic nerve compression, and meningitis. Intraventricular disease, as was the case in the above patient presentation, frequently results in obstructive hydrocephalus and its sequelae. Spinal neurocystirtcetosis is often asymptomatic, though may present as cord compression, meningitis, or lumbar arachoiditis.
PRESENTATION
Presentation of the disease depends on location and number of cysts, often with onset of symptoms approximately 3-5 years after initial infection. Cysts frequently begin the cycle of degeneration at that time, leading to an inflammatory response and edema. The most common presentation is seizure, headache, focal neurologic deficits, visual disturbances, and obstructive hydrocephalus though encephalitis and stroke are also possible. Diagnosis can be challenging, and is achieved via combination of CT, MRI, and serologic testing. At the time of diagnosis, ophthalmologic examination is required to exclude ocular disease before treatment with antihelmintic drugs, as the inflammatory response to treatment can lead to blindness.
TREATMENT
Treatment of neurocycticercosis begins with symptomatic care including treatment of pain, seizures, and intracranial hypertension. This may involve surgical treatment including ventricular fenestration, ventriculoperitoneal shunt placement, and excision of large lesions. All patients must be screened with formal ophthalmologic examination to assure the absence of ocular cysticercosis prior treatment with systemic antiparasitic agents. Disease specific treatment includes antihelmithic drugs including albendazole, plus or minus praziquantel though these are not recommended in all situations. Steroids, or steroid sparing agents are often given to prevent worsening of neurological symptoms due to edema and inflammation, as antiparasitic therapy is associated with worsening neurologic deficits and increased risk of hydrocephalus.
PROGNOSIS
Prognosis varies depending on site an number of lesions, though many lesions resolve spontaneously without treatment. Antihelmithic therapy is associated with lower recurrence of seizure and improves time to resolution. Outcomes are worse for those presenting with encephalitis, high cyst burden and subarachnoid neurocysticercosis. Those who present with intraventricular neurocysticercosis have a fair prognosis if they receive appropriate care and survive the acute phase of the disease.
CASE RESOLUTION
The patient had a ventriculostomy drain placed shortly after arrival to the tertiary care center. He was taken to the operating room several days thereafter for suboccipital craniotomy for microsurgical fenestration of the fourth ventricular cyst. He did have an intra-operative seizure and was started on anti-epileptics. The external ventricular drain was clamped and withdrawn several days later. The patient was discharged on an anti-epileptic with no further treatment. His neurologic exam had returned to baseline with 5 of 5 strength throughout and no further dysmetria.
Ophthalmologic exam demonstrated no evidence of ocular neurocysticercosis. Infectious disease consultation was obtained and broad workup for infectious agents was obtained. Further history revealed that in Guatemala he worked exclusively feeding pigs, chickens, and other farm animals for over 2 years. He immigrated to the USA 1 year and 8 months prior and had worked in a restaurant since.
No further antiparasitic medications was recommended.
Pathology of the intra-operative lesion demonstrated "fragments of Cysticercus cyst wall with foci of associated acute and chronic inflammation. No evidence of neoplasm"
The patient was lost to followup after discharge from the hospital.
AUTHOR: Victoria Leytin, MD is a Clinical Associate Professor of Emergency Medicine at Brown University Health.
PEER REVIEWER: Kristina McAteer, MD is a Clinical Associate Professor of Emergency Medicine at Brown University Health.
REFERENCES
CDC: Parasites - Cysticercosis. Resources for Health Professionals. CDC website. Reviewed October 22, 2020. Accessed May 9, 2023. https://www.cdc.gov/parasites/cysticercosis/health_professionals/index.html
Elsevier Point of Care: Clinical Overview - Cysticercosis. Updated July 30, 2025.
Garcia HH: Neurocysticercosis. Neurol Clin. 36(4):851-64, 2018