We use ultrasound for a multitude of procedures in the emergency department, including central and peripheral venous access, abscess drainage, and joint aspiration. Less common, but just as useful, is the use of ultrasound to help identify landmarks when performing a lumbar puncture (LP). While the traditional method of LP is based on palpating anatomical landmarks, this is becoming increasingly difficult as the patient population becomes more obese. It may also be difficult in patients who have abnormal spinal anatomy or in those who have had previous spinal surgery. When palpating anatomy is difficult, ultrasound can be a useful tool to help identify appropriate landmarks and increase your LP success rate…
Read MoreA 48 year-old female with idiopathic intracranial hypertension (IIH), with recent shunt removal, presented with increasing right eye vision loss over the last week, headache, and left-sided weakness. Her outpatient neuro-ophthalmologist referred her to the emergency department from clinic for a question of intracranial abscess, optic neuritis, or worsening IIH. She needed an MRI as soon as possible to rule-out these dangerous pathologies. A quick chart review showed that she has needed multiple central lines placed in the past, due to difficult IV access. The nurse was unable to place a peripheral IV…
Read MoreThis blog is meant to review some of the resources that helped me with this “hands-off” learning experience. There is no substitute for hands-on practice with ultrasound, but these sites were still an invaluable resource to my pandemic home ultrasound rotation…
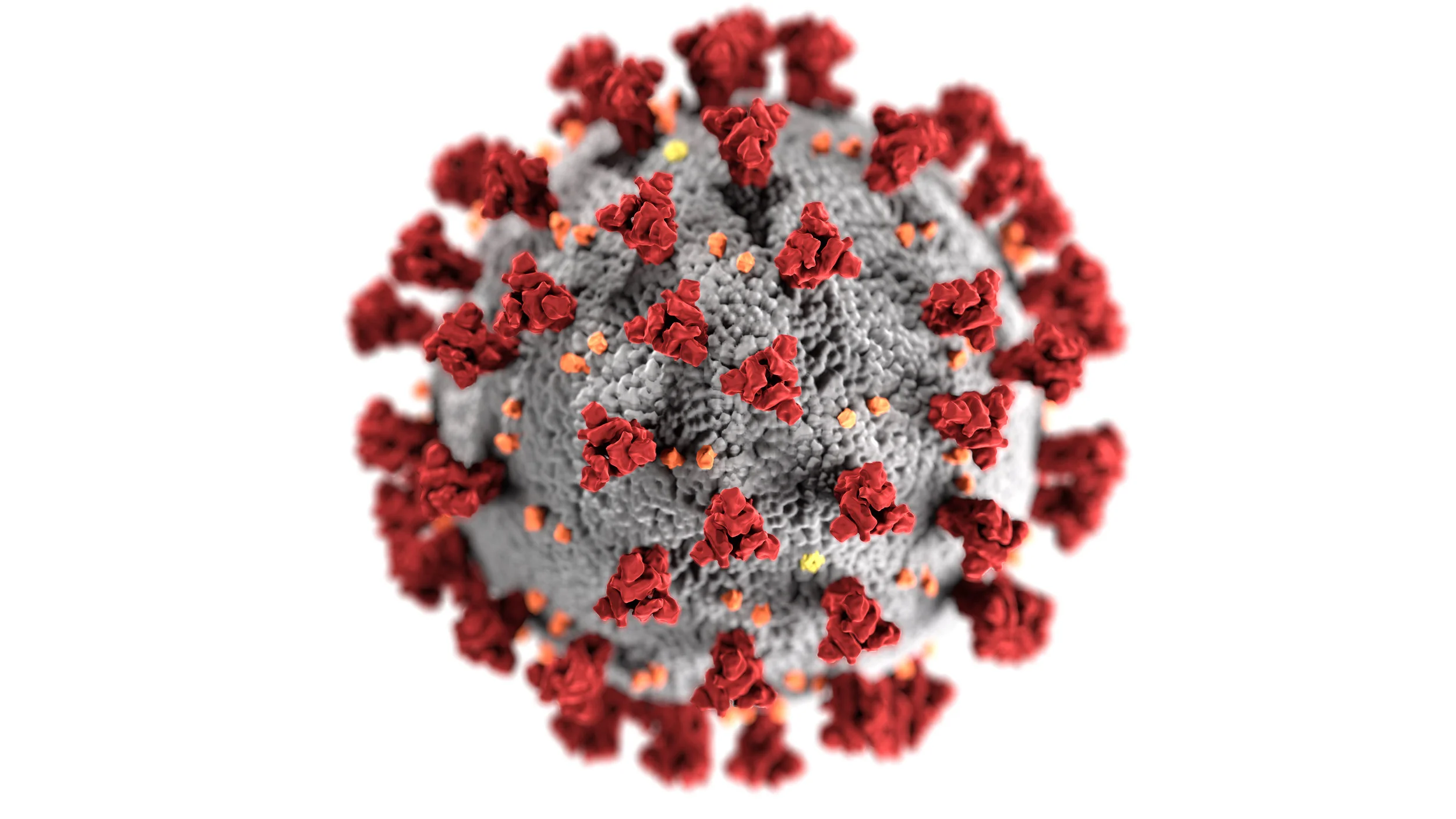
Read MoreSARS-CoV-2/COVID-19 is a novel coronavirus first identified in Wuhan, China in late 2019. There are many types of human coronavirus which cause mild symptoms, but COVID-19 is a new disease which has caused a global pandemic. In COVID-19 infection, there are specific findings seen on point-of-care lung ultrasound (LUS) which correlate to computed tomography findings. Thus, LUS may have an important role in the screening, diagnosis, and prognosis of patients presenting with an influenza like illness (ILI)…
Read MoreAn ex-full term six-week old male presented to the pediatric emergency department with three weeks of forceful, non-bloody, non-bilious emesis. He was having two to four episodes of vomiting that occurred after feeding. Three weeks prior, the patient had been transitioned from breast milk to formula, and attempts to thicken the formula by adding rice had not improved his vomiting. More recently, he had poor PO intake and his parents were concerned about his weight. He had no fevers, no change in number of wet diapers or stooling, and no other acute complaints…
Read More