Ultrasound Case of the Month: Hydatidiform Mole
CASE
A 32-year-old female with no significant past medical history presents to the emergency department with complaints of nausea, vomiting, and bloating. The patient reports her last menstrual period was about 2 months prior to presentation. She was evaluated one month ago, at which time pelvic ultrasound revealed an intrauterine gestation sac without a fetal pole or yolk sac, suspicious for early pregnancy failure. The patient subsequently developed vaginal bleeding, associated with abdominal cramping, nausea, and vomiting. She interpreted these symptoms as a miscarriage. The patient states that the vaginal bleeding has since subsided, but she endorses continued and progressive nausea, vomiting, and bloating. She is unable to tolerate oral intake. She denies fever, headache, abdominal pain, back pain, vaginal discharge/odor/pain, dysuria, or diarrhea.
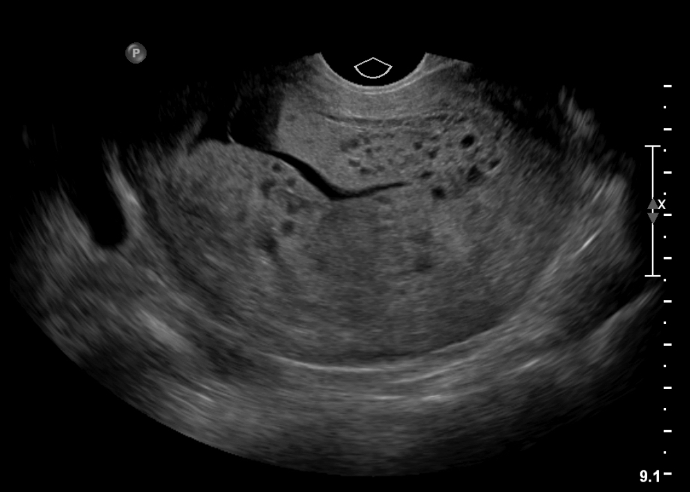
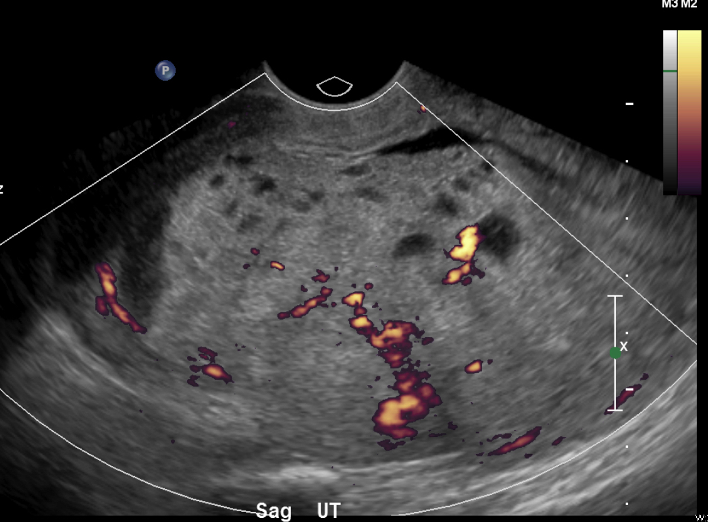
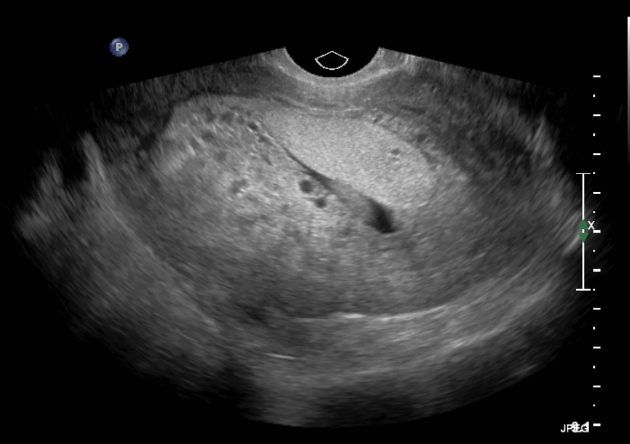
The following transvaginal ultrasound was performed:
Figure 1: Transvaginal and transabdominal ultrasound images with intra-uterine mass with cystic spaces and absence of fetal parts
DIAGNOSIS
Hydatidiform Mole
DISCUSSION
Molar pregnancies are frequently associated with B-hCG levels that are markedly elevated, causing the typical symptoms of nausea, vomiting, positive pregnancy test and missed menstruation. This patient was found to have B-hCG of 669,950.
In the emergency department, focused pelvic ultrasound is often used to evaluate first trimester vaginal bleeding, to confirm intra-uterine pregnancy, and to evaluate for suspected ectopic pregnancy. In general, a provider should attempt trans-abdominal ultrasound first, as it is less invasive.
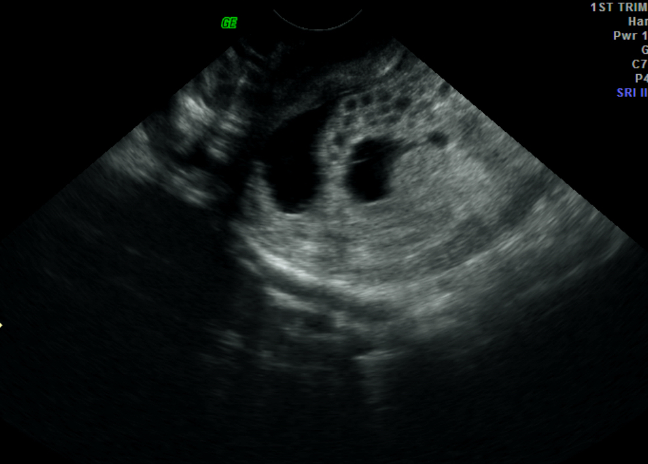
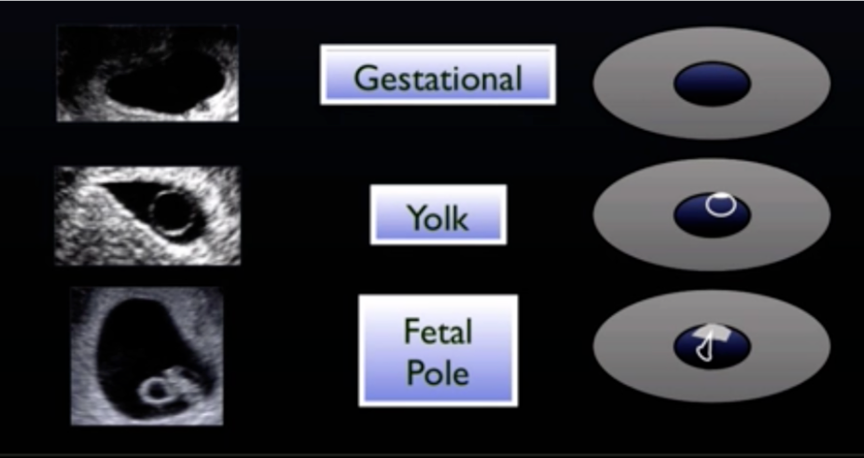
Intrauterine pregnancy can usually be seen at B-hCG levels > 1500 via trans-vaginal ultrasound and > 6500 via trans-abdominal ultrasound. [1] To confirm intra-uterine pregnancy, a gestational sac in addition to either a yolk sac or a fetal pole must be visualized. A gestational sac appears as an intra-uterine fluid collection embedded in the endometrium. A yolk sac appears as an echogenic ring (a “cheerio”) in the gestational sac. (Figure 2) In addition, these must be present within the uterus with an endomyometrial mantle of >5-7mm (measure from the gestational sac to the edge of the myometrium). If the gestational sac is closer than 5 mm from the edge of the myometrium, it is concerning for an interstitial pregnancy.
Figure 2: Ultrasound images of a gestational sac, yolk sac, and fetal pole. Courtesy of Dr. Kristin Dwyer, Director of Ultrasound Division of Brown Emergency Medicine
Trans-abdominal ultrasound should be performed when the patient has a full bladder. The curvilinear probe should be placed just superior to the pubic symphysis. The marker is pointed towards the patient’s head for sagittal/longitudinal view and to the patient’s right to obtain the transverse view.
In contrast, trans-vaginal ultrasound should be performed when the patient has an empty bladder. Remember to always use a sterile covering and gel over the endocavitary probe. Structures at the top of the screen are closer to the probe, whereas structures further away from the probe are along the bottom of the screen. The marker is facing up for the sagittal/longitudinal view and to the patient’s right for the transverse view. (Figure 3)
Figure 3: Representative depictions of the typical transverse and longitudinal views of pelvic structures when using the endocavitary ultrasound probe. Drawings courtesy of Dr. Erica Lash, Emergency Medicine Resident at Alpert Medical School of Brown University
The patient underwent a transabdominal and transvaginal ultrasound. The sagittal views of the uterus revealed the classic finding of a “bunch of grapes” appearance, with many cystic structures (and several larger cystic masses) within the uterus without any identifiable fetal pole or gestational sac. There is increased vascularity of the mass, which is also consistent with a diagnosis of hydatidiform mole.
Molar pregnancies can be challenging to diagnose, especially earlier in the first trimester. The gold standard of diagnosis is histologic evaluation of the uterine mass. Pre-evacuation, ultrasound is the preferred study of choice. The classic finding of intra-uterine cystic structures (bunch of grapes (earlier gestational age) or snowstorm sign (later gestational age)) results from abnormal proliferation and swelling of the trophoblastic villi. Characteristic ultrasound findings are more likely to be seen with complete moles rather than partial moles. In a complete mole, a fetus should not be present, in contrast to a partial mole where a fetus may be visualized. The sensitivity of ultrasound increases with gestational age, ranging from approximately 44-90%. It is important to note that some studies have found the detection rate of molar pregnancy (all types) to be less than 50% on routine ultrasound. Both the sensitivity and specificity increase when correlated with the hCG level. A higher level than expected based on gestational dates increases the likelihood of molar pregnancy.
TAKE-AWAYS
In the emergency department, focused pelvic ultrasound is often used to evaluate first trimester vaginal bleeding, to confirm intra-uterine pregnancy, and to evaluate for suspected ectopic pregnancy.
To confirm intra-uterine pregnancy, a gestational sac in addition to either a yolk sac or a fetal pole must be visualized.
Molar pregnancies can be challenging to diagnose. Pre-evacuation, ultrasound is the preferred study of choice.
Characteristic findings of intra-uterine cystic structures (“bunch of grapes”) or “snowstorm sign” can help with the diagnosis of hydatidiform mole.
Author: Dr. Erica Lash, MD is a fourth-year emergency medicine resident and chief resident at Brown University/Rhode Island Hospital.
Faculty Reviewer: Dr. Kristin Dwyer is the Director of Ultrasound Division of Brown Emergency Medicine
References
2. Fowler DJ, Lindsay I, Seckl MJ, Sebire NJ. Routine pre-evacuation ultrasound diagnosis of hydatidiform mole: experience of more than 1000 cases from a regional referral center. Ultrasound Obstet Gynecol 2006;27(1):56–60
3. https://radiopaedia.org/articles/complete-hydatidiform-mole