The EDUCATIONAL BLOG OF BROWN EMERGENCY MEDICINE RESIDENCY
WELCOME TO THE BROWN EM BLOG, THE OFFICIAL BLOG OF THE BROWN EMERGENCY MEDICINE RESIDENCY
-
WELCOME TO THE BROWN EM BLOG, THE OFFICIAL BLOG OF THE BROWN EMERGENCY MEDICINE RESIDENCY -
In this space we hope to enable Brown EM residents, fellows, faculty and medical students to publish educational blog posts, podcasts, discussion questions, journal reviews, procedural videos and images, or general musings to share with the medical community. This site is a #FOAMed friendly repository of knowledge. Please feel free to comment, like or share with others!
























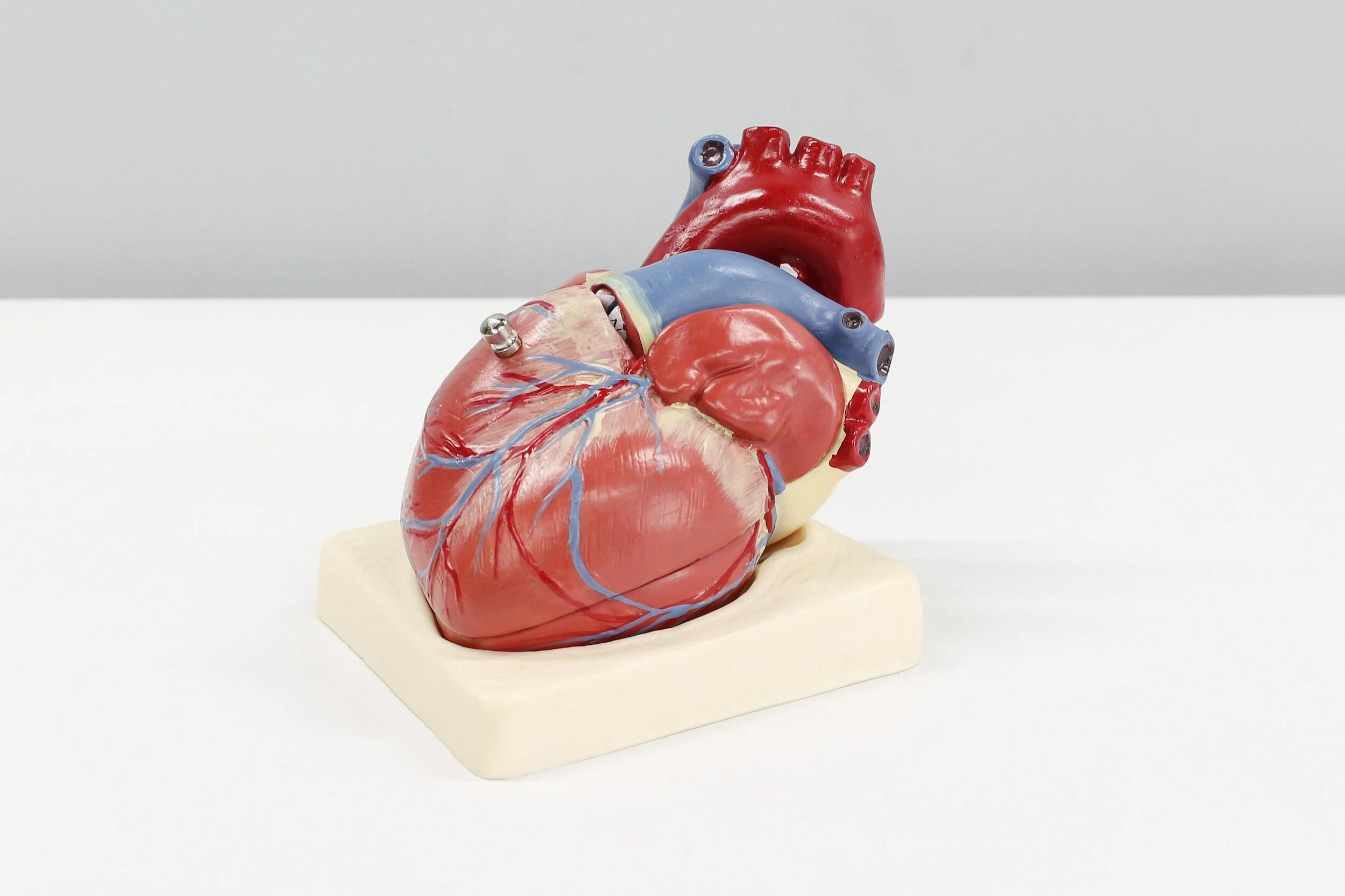































A 24-year-old healthy male presented to the emergency department (ED) with right ankle pain…